When ADHD and Eating Disorders Overlap: Why It All Feels So Messy and What Could Help
Ever had days when your body feels like it’s speaking a language you don’t quite get? Your brain says “eat,” but your body stays silent. Or you plan to eat “later,” then suddenly it’s 8 p.m. and you’re starving, grabbing whatever’s easy. If you live with ADHD, this might sound familiar.
Living with ADHD can present unique challenges, and for some people, it may also intersect with disordered eating patterns. Understanding how ADHD symptoms, like impulsivity, inattentiveness, or difficulty with emotional regulation, can affect eating behaviors is an important step toward developing effective coping strategies and seeking support.
In this blog, we’ll explore the ways ADHD and eating disorders can overlap, highlight common patterns, and offer practical strategies for managing both. More than you might think, ADHD and disordered-eating or full eating-disorder patterns often show up together. For many people, it’s not about being “broken” or doing something wrong. It’s about how ADHD changes the way your brain, body, and emotions communicate with each other.
What ADHD Does to Body Awareness and Eating Patterns
First, I think it is important to get a clear understanding of how ADHD can impact body awareness and eating patterns. ADHD does not just affect focus or attention. It also influences the way a person notices internal cues, organizes daily routines, responds to emotions, and moves through their day. All of these pieces directly shape how someone experiences hunger, fullness, eating habits, and their connection to their body. While ADHD itself does not cause eating disorders, certain symptoms can increase vulnerability. Understanding this foundation makes it easier to see how certain ADHD traits can gradually shift into patterns that look or feel like disordered eating.
Hunger cues can get fuzzy
When you have ADHD, interoceptive awareness, tuning into subtle internal signals such as hunger, fullness, or body stress can be harder. Many people describe it like their internal antenna is turned down. They only notice hunger when it is very strong or when food happens to be nearby. This makes regular balanced eating difficult and can lead to cycles of ignoring hunger followed by overeating. Some research even suggests that people with ADHD may have more difficulty sensing what is happening inside their bodies, including hunger and fullness cues.
Executive functioning makes meal planning difficult
Cooking a nutritious meal involves many steps. You have to remember to shop, choose what to make, prep ingredients, cook, and clean up. For people with ADHD, that chain of tasks can feel overwhelming. Skipping meals, relying on convenience foods, or eating only when something quick is available becomes more of a survival strategy than a choice. This kind of irregular eating rhythm often overlaps with disordered eating patterns.
Impulsivity and the brain's reward system create challenges
ADHD often comes with a brain that searches for quick reward. Food, especially sugary or high energy foods, can give a fast boost. That makes impulsive or binge type eating more likely for some people. Emotional triggers such as stress, shame, or loneliness can also blend with impulsivity and low self regulation. When food becomes one of the only ways to soothe or get quick relief, the pattern becomes harder to break.
Sensitive emotions and a fear of rejection add another layer
Many people with ADHD experience intense emotional discomfort when they feel criticized or rejected. This can lead to restrictive eating, secretive bingeing, or feeling stuck in cycles of shame. When shame becomes part of the eating pattern, healing becomes more complicated because the struggle is often about deeper emotional pain, not just food.
What the Research Says:
A large meta-analysis found people with Attention Deficit Hyperactivity Disorder (ADHD) are about 3.8 times more likely to be diagnosed with an eating disorder (ED) compared with people without ADHD. PubMed
Within that same analysis, the increased risk held across different ED diagnoses: about 4.3 times higher for Anorexia Nervosa (AN), 5.7 times higher for Bulimia Nervosa (BN), and 4.1 times higher for Binge Eating Disorder (BED). PubMed
In a matched cohort study of children and adolescents with ADHD, 31.43% screened “at risk” for an eating disorder (via EAT-26), compared with 12.14% of matched controls without ADHD, showing a notably higher risk in youth. pmc.ncbi.nlm.nih.gov+1
Community-based research among adolescents found that those with ADHD symptoms had significantly higher rates of disordered-eating behaviors compared to their peers without ADHD, supporting that this overlap is not limited to clinical or treatment-seeking samples. However, it is also worth noting when researchers adjusted for other factors (anxiety, substance use, etc.), the strength of the association lessened. PubMed+1
The mechanisms (why/ how) are still under investigation. Shared genetics, neurobiological reward pathways (dopamine), executive‑function challenges, emotional regulation, interoceptive awareness all play possible roles. PubMed+2ScienceDirect+
Taken together, these findings make a strong case that ADHD significantly increases the likelihood of disordered eating or a full eating disorder, well beyond what would be expected by random chance.
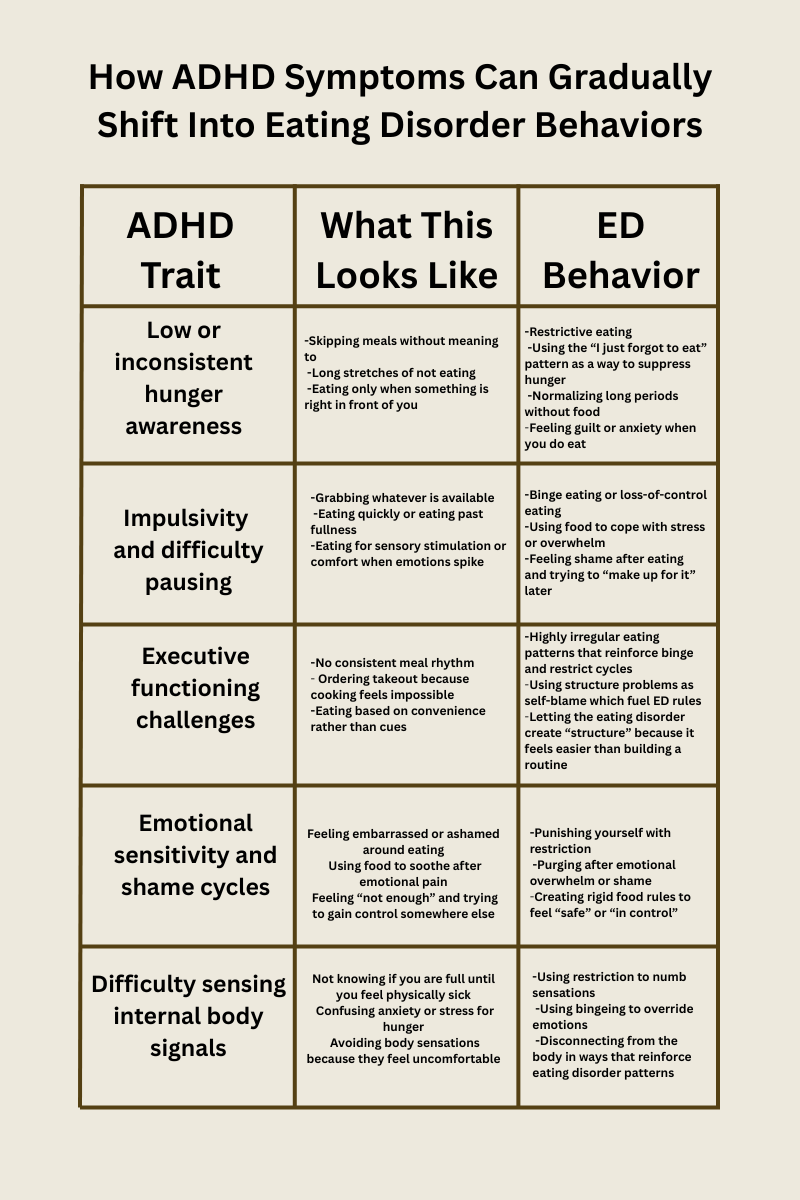
How ADHD Symptoms Can Gradually Shift Into Eating Disorder Behaviors
Eating disorders do not usually show up suddenly. Instead they often grow from patterns that begin as ADHD traits coping strategies or moments of overwhelm. Over time those same patterns can shift into something more rigid or more painful.
Below is a gentle map of how this progression can happen.
Need for stimulation or reward
Another factor to consider is that a person with ADHD may move toward foods that offer quick pleasure when bored or seeking comfort.
Over time ED behaviors can take advantage of this by using food for emotional regulation or using restriction for emotional numbness creating rigid patterns that are hard to escape.
This progression does not happen because someone chooses an eating disorder. It happens because ADHD traits create vulnerabilities that eating disorders latch onto.
Nuances: The Spectrum of Eating-Related Experiences
It’s important to recognize that the relationship between ADHD and eating behaviors exists on a spectrum—there’s no single experience that applies to everyone. Some individuals may struggle with binge eating or emotional eating, where impulsivity and difficulty regulating emotions play a role. Others may experience restrictive or selective eating, sometimes linked to sensory sensitivities or challenges with interoceptive awareness (not noticing hunger or fullness).
Examples of eating-related patterns seen in people with ADHD may include:
Binge eating or emotional eating in response to stress or impulsivity
Restrictive eating due to sensory sensitivities or routine disruptions
Irregular or missed meals from inattention or executive-function challenges
Selective eating patterns, sometimes overlapping with ARFID
Additionally, eating patterns can fluctuate over time, depending on stress, routine, sleep, or co-occurring conditions such as anxiety or depression. ADHD symptoms may amplify certain behaviors at some points in life and less so at others.
Research supports that ADHD symptoms can contribute to a variety of eating patterns, but experiences vary widely among individuals.
Understanding this variability helps to avoid overgeneralization, validates diverse experiences, and emphasizes that individualized strategies, rather than one-size-fits-all approaches, are most effective for supporting both ADHD management and healthy eating behaviors.
What about ARFID?
Avoidant/Restrictive Food Intake Disorder (ARFID) and ADHD often overlap because both involve sensory sensitivities, low interoceptive awareness, and executive functioning challenges. For many with ADHD, textures, smells, or temperatures can feel overwhelming, while irregular hunger cues or difficulty trying new foods make eating harder. This combination can contribute to restrictive patterns that go beyond “picky eating.”
When Eating Disorders Take Advantage of ADHD Symptoms
This is one of the most important pieces people often do not get told. Eating disorders frequently build themselves around the exact symptoms that make ADHD difficult.
If you are forgetful, the eating disorder uses that to push restriction.
If emotions hit hard, the eating disorder offers bingeing or purging as a release.
If planning meals feels impossible, the eating disorder steps in with rigid rules.
It becomes surprisingly easy to mistake an eating disorder pattern for an ADHD quirk. And once those wires get crossed, untangling them requires compassion and clarity.
Why This Matters
Understanding the overlap between ADHD and eating disorders helps us see that for many people, disordered eating is not just about food. It is about brain wiring, emotional experiences, body awareness, and the rhythm of daily life.
This means:
Early screening is important for anyone with ADHD experiencing eating challenges.
Treatment should consider both ADHD and eating behaviors, not just one.
Recovery is possible with structure, emotional support, and ADHD friendly strategies.
Quick Takeaways: ADHD & Eating Disorders
People with ADHD are at higher risk for disordered eating, especially binge eating or bulimia, but not everyone with ADHD will experience these challenges. In fact, many people with ADHD will not experience an eating disorder.
Traits like impulsivity, inattention, emotional regulation difficulties, and sensory sensitivities can influence eating patterns.
The exact reasons ADHD and eating disorders overlap aren’t fully understood; likely factors include brain reward pathways, executive-function differences, and awareness of internal cues.
Individual experiences vary, so personalized support and treatment addressing both ADHD and eating behaviors is key.
References:
Instanes, J. T., Klungsoyr, K., Halmøy, A., Fasmer, O. B., & Haavik, J. (2016). The risk of eating disorders comorbid with attention deficit/hyperactivity disorder: A systematic review and meta-analysis. International Journal of Eating Disorders, 49(10), 1045–1057. https://pubmed.ncbi.nlm.nih.gov/27859581/
Jahrami, H., AlAnsari, A. M., Janahi, A. I., Janahi, A. K., Darraj, L. R., & Faris, M. (2021). The risk of eating disorders among children and adolescents with attention deficit hyperactivity disorder: Results of a matched cohort study. International Journal of Pediatrics and Adolescent Medicine, 8(2), 102–106. https://pmc.ncbi.nlm.nih.gov/articles/PMC8144858/
Cortese, S., & Vincenzi, B. (2017). Attention deficit hyperactivity disorder symptoms and psychological comorbidity in eating disorder patients. Psychiatry Research, 254, 70–76. https://pubmed.ncbi.nlm.nih.gov/28534123/
Nazar, B. P. D., Morales-Alvarez, C., & Newlove-Delgado, T. (2017). Attention deficit/hyperactivity disorder and eating disorders across the lifespan: A systematic review of the literature. European Psychiatry, 45, 27–36. https://pubmed.ncbi.nlm.nih.gov/27693587/
Nobis, M., Laghi, F., Brunetti, C., Cabaleiro, L., Hernández-Martínez, C., & Jansen, A. (2022). The association between eating disorders and mental health: An umbrella review. Journal of Eating Disorders, 10, Article 132. https://jeatdisord.biomedcentral.com/articles/10.1186/s40337-022-00725-4