Why Motivation Is Not the Problem Especially for ADHD Brains
Many people who think they lack motivation are actually dealing with executive dysfunction. This post explains why starting tasks can feel impossible, how shame and avoidance create a self-reinforcing cycle, and why the real solution is support, not self-criticism. Understanding what is happening in your brain can replace frustration with clarity and help you move forward with more effective strategies.
You wake up determined to clean the house.
You want to do it. You plan to do it. You even have time.
But when you start, your brain suddenly shows you everything at once. Dishes. Laundry. Clutter. Emails. The thing you forgot yesterday. The thing you should do before cleaning. The thing you should research before that.
The task instantly feels enormous. Your body slows down. You check your phone for just a second. Maybe you scroll. Maybe you wander. Maybe you organize one drawer instead.
Later nothing is done. And the thought appears
Why can I not just do it? I have no motivation.
But what if motivation was never the problem?
ADHD affects how the brain regulates attention, effort, and activation, not how much someone cares. What looks like a lack of motivation is often the nervous system struggling to initiate action.
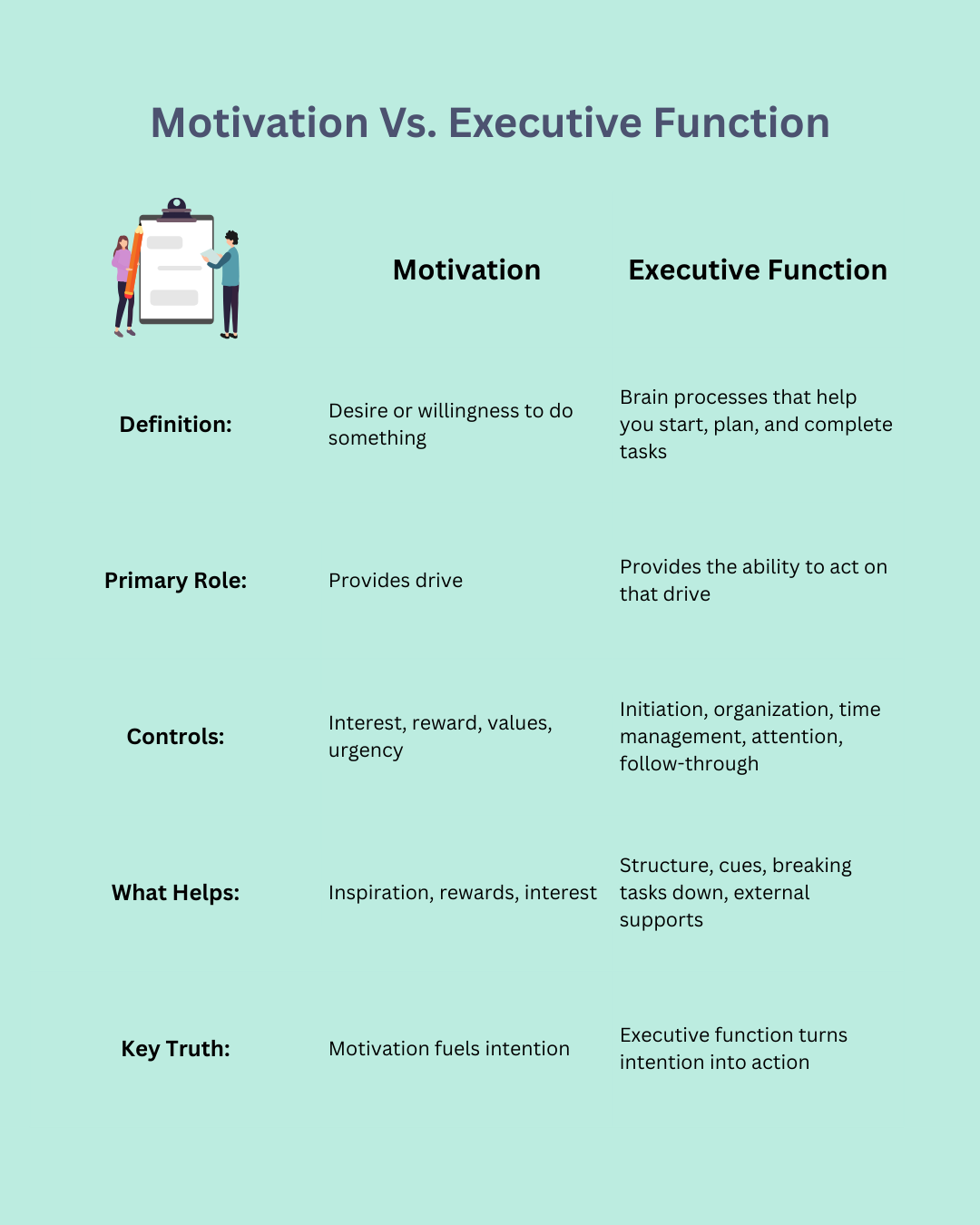
Motivation vs Executive Function
Most of us were taught a simple formula:
If you care you will do it.
This formula works for people whose executive functioning system runs smoothly. Executive functions are the brain’s management processes responsible for starting tasks, organizing steps, shifting attention, managing time, and sustaining effort.
When those systems struggle, the real equation looks more like:
Care deeply → Brain overload = Stuck
You are not failing to act because you do not want to or your lack motivation. You are stuck because the system that translates intention into action gets jammed. Motivation determines whether you want to do something. Executive function determines whether you can start and follow through.
What Executive Dysfunction Really Feels Like
From the outside it can look like procrastination. On the inside it often feels like paralysis.
Many people describe it as knowing exactly what they need to do but feeling unable to begin, like their brain is pressing the brake pedal while they are trying to move forward. They may sit in discomfort watching time pass, they may pace or start doing an unrelated task, while wanting to act but feeling mentally blocked.
This is why it is important to clarify that this is not a motivation problem.
It is a regulation problem. Executive dysfunction is a neurological regulation issue, not a character flaw.
Why Shame Makes Everything Harder
Another obstacle that often gets in the way of people being able to follow through on tasks is shame.
Some people will argue that “tough love” is way they can motivate themselves; however, it is important to note that shame blocks action.
When your internal voice says things like I am lazy, I should be able to do this, or What is wrong with me, your nervous system interprets that as threat. When the brain detects threat, it shifts resources away from planning, focus, and initiation, and shifts focus towards a survival mode: fight, flight, freeze or fawn response.
In other words, shame shuts down the exact skills you need in order to start.
The Hidden Truth About “Unmotivated” People
Most people who think they lack motivation actually care too much, not too little.
They often carry constant internal pressure. They mentally track unfinished tasks, worry about falling behind, and hold themselves to very high standards. That pressure builds until the brain becomes overloaded and overwhelmed and stops initiating.
This is not refusal, this is their nervous system trying to protect them.
Once people understand this is not a character flaw, they often begin to recognize a pattern they have been stuck in for years.
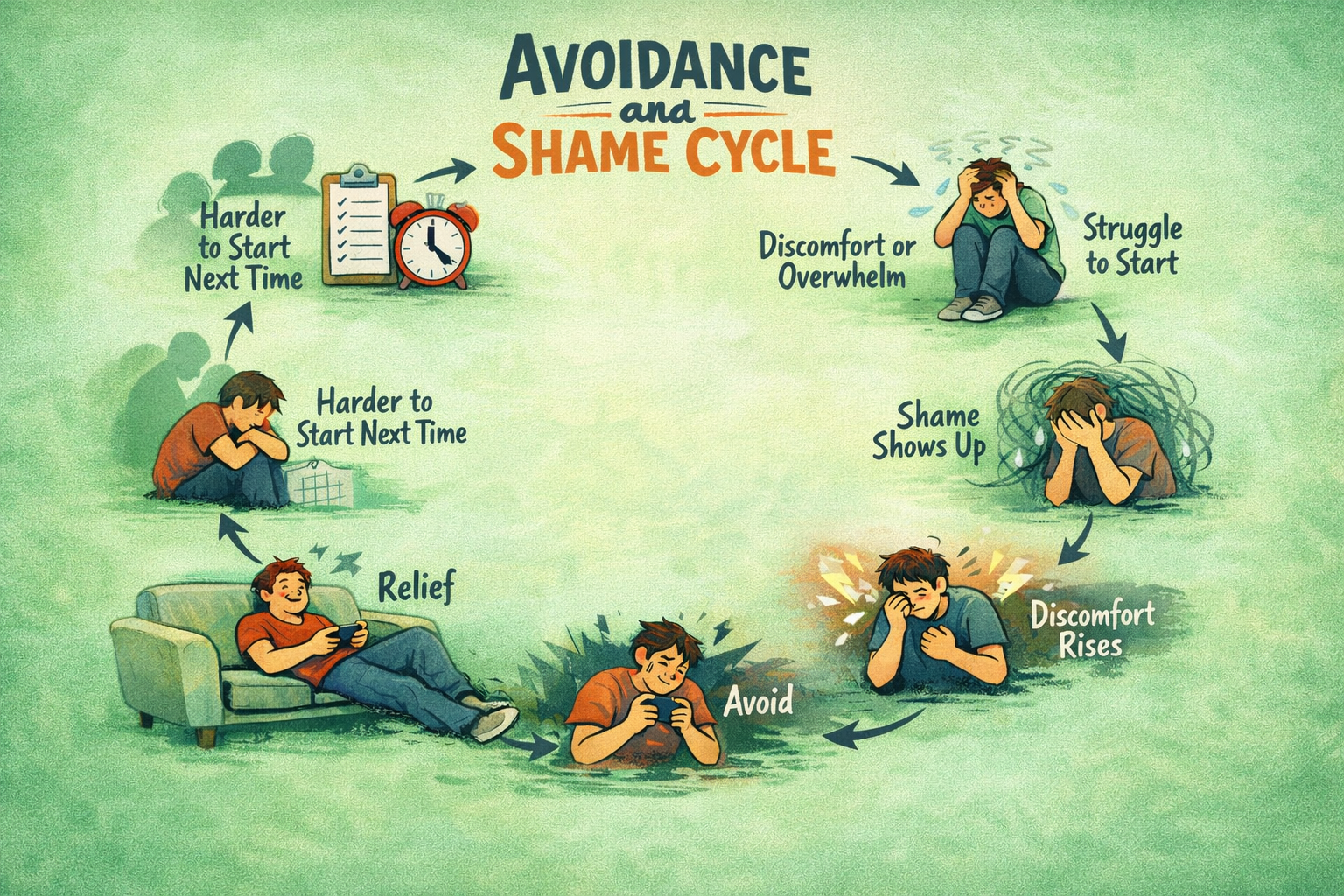
A Pattern You May Recognize
Once people realize this is not a character flaw, they often start noticing a pattern they have experienced over and over but never had language for. It is not random. It follows a predictable loop.
For example, imagine you notice the dishes in the sink. You tell yourself you should do them. Almost immediately you feel resistance in your body. The task suddenly feels bigger than it actually is. You think about how long it will take, how tired you are, how many dishes there are. Starting feels hard. Then the thoughts show up. Why am I like this? This is so simple. I should have done this already.
Now the discomfort is stronger, not weaker. So you walk away and check your phone or sit down for a minute. The moment you step away, you feel a small wave of relief. The pressure drops.
Later, though, the dishes are still there. And now the relief has been replaced with more shame, more dread, and a stronger urge to avoid it next time.
This is the cycle.
The Avoidance Cycle
Many people with ADHD traits find themselves in a predictable loop.
When a task comes up, it can trigger feelings of discomfort or overwhelm, making it hard to get started. As shame creeps in, that discomfort grows, leading to avoidance. While avoiding provides brief relief, the shame lingers and builds, making it even harder to tackle the next task. This cycle can repeat over and over, showing how avoidance and shame reinforce each other.
Avoidance is not proof that you do not care. It is your brain trying to reduce discomfort. Distraction is a short term relief strategy that calms the nervous system temporarily. But afterward the task is still there, however now it is layered with guilt.
Shame acts like glue in this cycle. It keeps you stuck while convincing you the problem is your character.
How to Tell It Is Executive Dysfunction Not Laziness
There is an important difference between not wanting to do something and being unable to start.
Signs that executive functioning may be the issue include difficulty starting even tasks you care about, doing well under urgency but struggling without deadlines, starting strong but not sustaining momentum, or finding it easier to complete tasks when someone else is present.
Laziness means you do not want to do it.
Executive dysfunction means you want to but your brain is struggling to turn that want into action.
This distinction matters because the way we approach these two things are completely different.
What Actually Helps
Before strategies work, it helps to understand that difficulty starting is not resistance. It is a regulation barrier. If motivation is not the problem, pushing harder will not fix it. What helps is reducing friction between intention and action.
Creating external structure, breaking tasks into small steps, paying attention to sensory input, and practicing supportive self-talk can make it easier to help your brain take action and follow through.
One of the most powerful shifts is changing your internal question from:
Why can I not do this?
to
What would make this easier to start or what is one thing I can do for the next 5 minutes
That question moves you from shame into problem solving, and problem solving is where momentum begins.
Take Away
Struggling to start tasks does not mean you are lazy.
It does not mean you lack discipline.
It does not mean you do not care.
Often it means your brain needs different supports than the ones you were taught to use. This distinction matters not just emotionally but practically.
Understanding executive dysfunction does not mean lowering expectations. It means changing the strategies we use to address what is actually getting in the way. When we do that, people often realize the issue was never an inability to follow through. They are far more capable than they have been led to believe.
If this resonates with you, there is nothing wrong with you. You may simply be using motivation-based solutions for a regulation-based difficulty.
And those require entirely different tools.
When ADHD and Eating Disorders Overlap: Why It All Feels So Messy and What Could Help
ADHD and eating disorders often overlap in ways that many people do not expect. ADHD impacts body awareness, hunger cues, emotional regulation, and daily routines, which can make consistent eating patterns difficult. Over time, these everyday ADHD experiences can gradually shift into disordered eating or full eating disorder behaviors, especially when impulsivity, rejection sensitivity, or executive functioning struggles are part of the picture.
Research shows people with ADHD are significantly more likely to develop eating disorders, including anorexia, bulimia, and binge eating disorder. The blog explores how this connection forms, how eating disorders can take advantage of ADHD symptoms, and why understanding this link is essential for early support, compassionate treatment, and sustainable recovery.
Ever had days when your body feels like it’s speaking a language you don’t quite get? Your brain says “eat,” but your body stays silent. Or you plan to eat “later,” then suddenly it’s 8 p.m. and you’re starving, grabbing whatever’s easy. If you live with ADHD, this might sound familiar.
Living with ADHD can present unique challenges, and for some people, it may also intersect with disordered eating patterns. Understanding how ADHD symptoms, like impulsivity, inattentiveness, or difficulty with emotional regulation, can affect eating behaviors is an important step toward developing effective coping strategies and seeking support.
In this blog, we’ll explore the ways ADHD and eating disorders can overlap, highlight common patterns, and offer practical strategies for managing both. More than you might think, ADHD and disordered-eating or full eating-disorder patterns often show up together. For many people, it’s not about being “broken” or doing something wrong. It’s about how ADHD changes the way your brain, body, and emotions communicate with each other.
What ADHD Does to Body Awareness and Eating Patterns
First, I think it is important to get a clear understanding of how ADHD can impact body awareness and eating patterns. ADHD does not just affect focus or attention. It also influences the way a person notices internal cues, organizes daily routines, responds to emotions, and moves through their day. All of these pieces directly shape how someone experiences hunger, fullness, eating habits, and their connection to their body. While ADHD itself does not cause eating disorders, certain symptoms can increase vulnerability. Understanding this foundation makes it easier to see how certain ADHD traits can gradually shift into patterns that look or feel like disordered eating.
Hunger cues can get fuzzy
When you have ADHD, interoceptive awareness, tuning into subtle internal signals such as hunger, fullness, or body stress can be harder. Many people describe it like their internal antenna is turned down. They only notice hunger when it is very strong or when food happens to be nearby. This makes regular balanced eating difficult and can lead to cycles of ignoring hunger followed by overeating. Some research even suggests that people with ADHD may have more difficulty sensing what is happening inside their bodies, including hunger and fullness cues.
Executive functioning makes meal planning difficult
Cooking a nutritious meal involves many steps. You have to remember to shop, choose what to make, prep ingredients, cook, and clean up. For people with ADHD, that chain of tasks can feel overwhelming. Skipping meals, relying on convenience foods, or eating only when something quick is available becomes more of a survival strategy than a choice. This kind of irregular eating rhythm often overlaps with disordered eating patterns.
Impulsivity and the brain's reward system create challenges
ADHD often comes with a brain that searches for quick reward. Food, especially sugary or high energy foods, can give a fast boost. That makes impulsive or binge type eating more likely for some people. Emotional triggers such as stress, shame, or loneliness can also blend with impulsivity and low self regulation. When food becomes one of the only ways to soothe or get quick relief, the pattern becomes harder to break.
Sensitive emotions and a fear of rejection add another layer
Many people with ADHD experience intense emotional discomfort when they feel criticized or rejected. This can lead to restrictive eating, secretive bingeing, or feeling stuck in cycles of shame. When shame becomes part of the eating pattern, healing becomes more complicated because the struggle is often about deeper emotional pain, not just food.
What the Research Says:
A large meta-analysis found people with Attention Deficit Hyperactivity Disorder (ADHD) are about 3.8 times more likely to be diagnosed with an eating disorder (ED) compared with people without ADHD. PubMed
Within that same analysis, the increased risk held across different ED diagnoses: about 4.3 times higher for Anorexia Nervosa (AN), 5.7 times higher for Bulimia Nervosa (BN), and 4.1 times higher for Binge Eating Disorder (BED). PubMed
In a matched cohort study of children and adolescents with ADHD, 31.43% screened “at risk” for an eating disorder (via EAT-26), compared with 12.14% of matched controls without ADHD, showing a notably higher risk in youth. pmc.ncbi.nlm.nih.gov+1
Community-based research among adolescents found that those with ADHD symptoms had significantly higher rates of disordered-eating behaviors compared to their peers without ADHD, supporting that this overlap is not limited to clinical or treatment-seeking samples. However, it is also worth noting when researchers adjusted for other factors (anxiety, substance use, etc.), the strength of the association lessened. PubMed+1
The mechanisms (why/ how) are still under investigation. Shared genetics, neurobiological reward pathways (dopamine), executive‑function challenges, emotional regulation, interoceptive awareness all play possible roles. PubMed+2ScienceDirect+
Taken together, these findings make a strong case that ADHD significantly increases the likelihood of disordered eating or a full eating disorder, well beyond what would be expected by random chance.
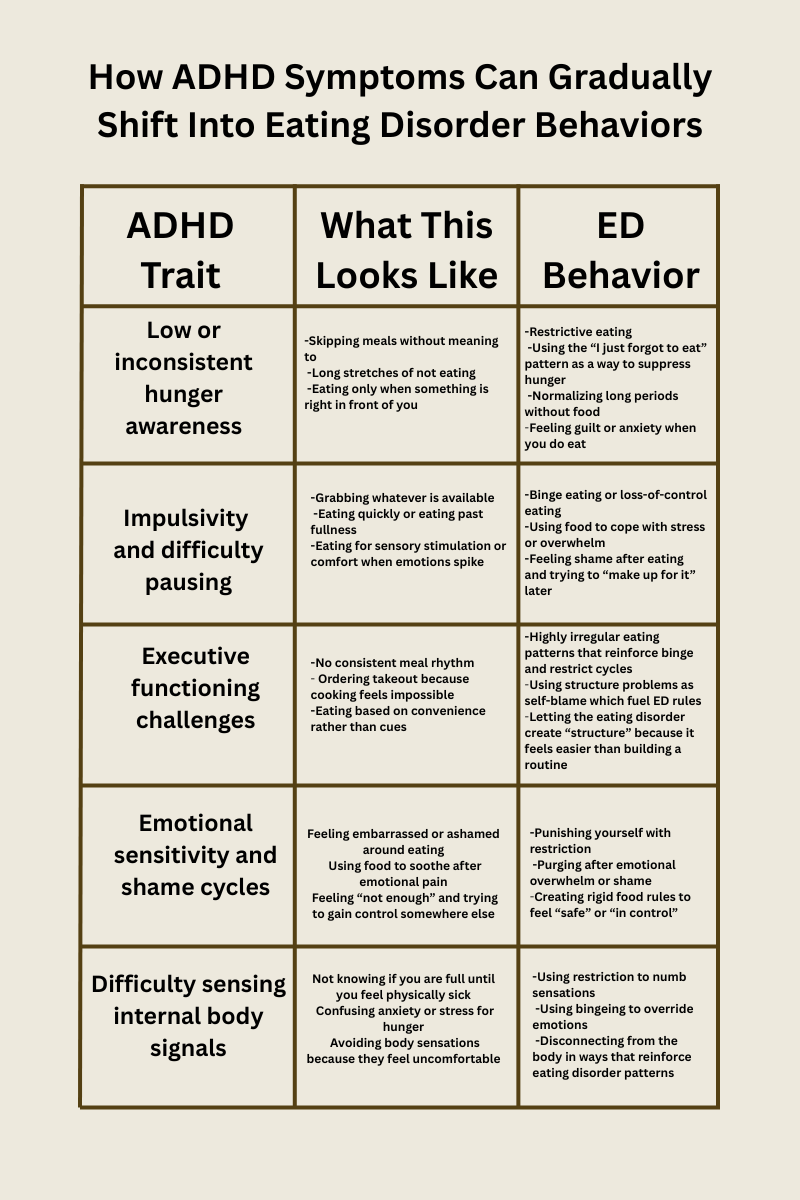
How ADHD Symptoms Can Gradually Shift Into Eating Disorder Behaviors
Eating disorders do not usually show up suddenly. Instead they often grow from patterns that begin as ADHD traits coping strategies or moments of overwhelm. Over time those same patterns can shift into something more rigid or more painful.
Below is a gentle map of how this progression can happen.
Need for stimulation or reward
Another factor to consider is that a person with ADHD may move toward foods that offer quick pleasure when bored or seeking comfort.
Over time ED behaviors can take advantage of this by using food for emotional regulation or using restriction for emotional numbness creating rigid patterns that are hard to escape.
This progression does not happen because someone chooses an eating disorder. It happens because ADHD traits create vulnerabilities that eating disorders latch onto.
Nuances: The Spectrum of Eating-Related Experiences
It’s important to recognize that the relationship between ADHD and eating behaviors exists on a spectrum—there’s no single experience that applies to everyone. Some individuals may struggle with binge eating or emotional eating, where impulsivity and difficulty regulating emotions play a role. Others may experience restrictive or selective eating, sometimes linked to sensory sensitivities or challenges with interoceptive awareness (not noticing hunger or fullness).
Examples of eating-related patterns seen in people with ADHD may include:
Binge eating or emotional eating in response to stress or impulsivity
Restrictive eating due to sensory sensitivities or routine disruptions
Irregular or missed meals from inattention or executive-function challenges
Selective eating patterns, sometimes overlapping with ARFID
Additionally, eating patterns can fluctuate over time, depending on stress, routine, sleep, or co-occurring conditions such as anxiety or depression. ADHD symptoms may amplify certain behaviors at some points in life and less so at others.
Research supports that ADHD symptoms can contribute to a variety of eating patterns, but experiences vary widely among individuals.
Understanding this variability helps to avoid overgeneralization, validates diverse experiences, and emphasizes that individualized strategies, rather than one-size-fits-all approaches, are most effective for supporting both ADHD management and healthy eating behaviors.
What about ARFID?
Avoidant/Restrictive Food Intake Disorder (ARFID) and ADHD often overlap because both involve sensory sensitivities, low interoceptive awareness, and executive functioning challenges. For many with ADHD, textures, smells, or temperatures can feel overwhelming, while irregular hunger cues or difficulty trying new foods make eating harder. This combination can contribute to restrictive patterns that go beyond “picky eating.”
When Eating Disorders Take Advantage of ADHD Symptoms
This is one of the most important pieces people often do not get told. Eating disorders frequently build themselves around the exact symptoms that make ADHD difficult.
If you are forgetful, the eating disorder uses that to push restriction.
If emotions hit hard, the eating disorder offers bingeing or purging as a release.
If planning meals feels impossible, the eating disorder steps in with rigid rules.
It becomes surprisingly easy to mistake an eating disorder pattern for an ADHD quirk. And once those wires get crossed, untangling them requires compassion and clarity.
Why This Matters
Understanding the overlap between ADHD and eating disorders helps us see that for many people, disordered eating is not just about food. It is about brain wiring, emotional experiences, body awareness, and the rhythm of daily life.
This means:
Early screening is important for anyone with ADHD experiencing eating challenges.
Treatment should consider both ADHD and eating behaviors, not just one.
Recovery is possible with structure, emotional support, and ADHD friendly strategies.
Quick Takeaways: ADHD & Eating Disorders
People with ADHD are at higher risk for disordered eating, especially binge eating or bulimia, but not everyone with ADHD will experience these challenges. In fact, many people with ADHD will not experience an eating disorder.
Traits like impulsivity, inattention, emotional regulation difficulties, and sensory sensitivities can influence eating patterns.
The exact reasons ADHD and eating disorders overlap aren’t fully understood; likely factors include brain reward pathways, executive-function differences, and awareness of internal cues.
Individual experiences vary, so personalized support and treatment addressing both ADHD and eating behaviors is key.
References:
Instanes, J. T., Klungsoyr, K., Halmøy, A., Fasmer, O. B., & Haavik, J. (2016). The risk of eating disorders comorbid with attention deficit/hyperactivity disorder: A systematic review and meta-analysis. International Journal of Eating Disorders, 49(10), 1045–1057. https://pubmed.ncbi.nlm.nih.gov/27859581/
Jahrami, H., AlAnsari, A. M., Janahi, A. I., Janahi, A. K., Darraj, L. R., & Faris, M. (2021). The risk of eating disorders among children and adolescents with attention deficit hyperactivity disorder: Results of a matched cohort study. International Journal of Pediatrics and Adolescent Medicine, 8(2), 102–106. https://pmc.ncbi.nlm.nih.gov/articles/PMC8144858/
Cortese, S., & Vincenzi, B. (2017). Attention deficit hyperactivity disorder symptoms and psychological comorbidity in eating disorder patients. Psychiatry Research, 254, 70–76. https://pubmed.ncbi.nlm.nih.gov/28534123/
Nazar, B. P. D., Morales-Alvarez, C., & Newlove-Delgado, T. (2017). Attention deficit/hyperactivity disorder and eating disorders across the lifespan: A systematic review of the literature. European Psychiatry, 45, 27–36. https://pubmed.ncbi.nlm.nih.gov/27693587/
Nobis, M., Laghi, F., Brunetti, C., Cabaleiro, L., Hernández-Martínez, C., & Jansen, A. (2022). The association between eating disorders and mental health: An umbrella review. Journal of Eating Disorders, 10, Article 132. https://jeatdisord.biomedcentral.com/articles/10.1186/s40337-022-00725-4
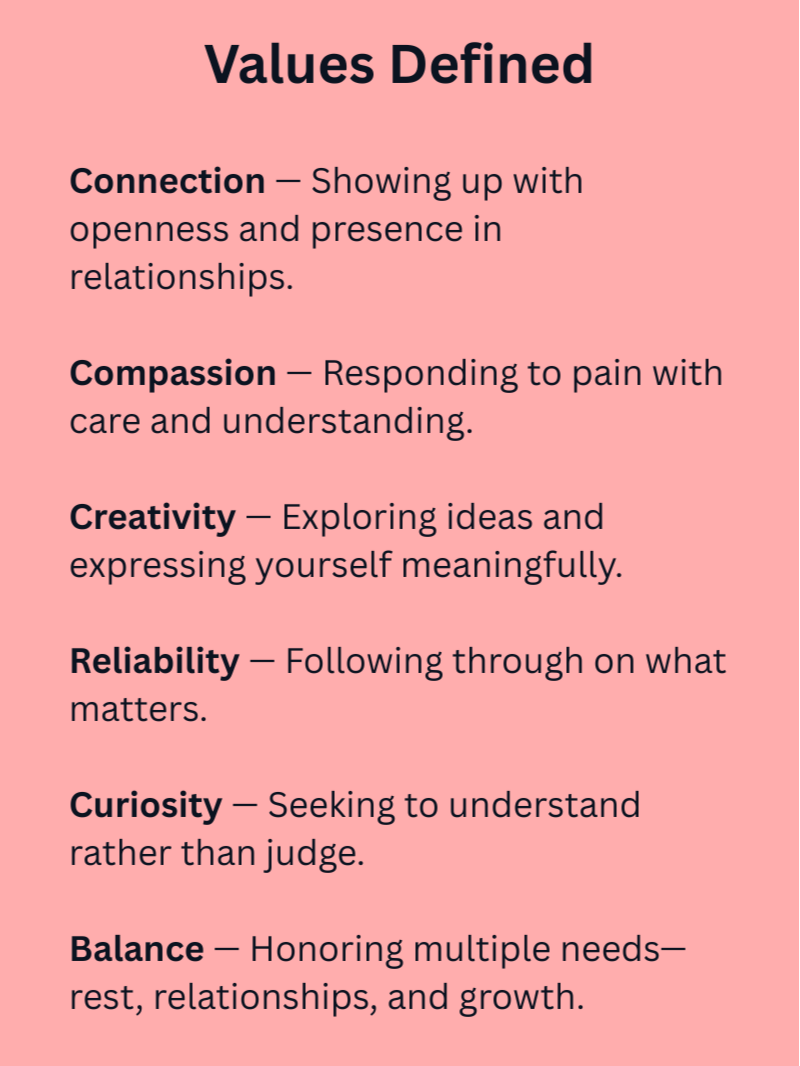
Values: Your Inner Compass
Life can feel messy and unpredictable, leaving us unsure of which direction to take. This post explores how values act as a personal compass, guiding your decisions, clarifying priorities, and helping you live intentionally. Learn how to define your values in your own words, identify your core values, understand the messages behind your emotions, and take practical steps toward a values-aligned life.
Life can feel unpredictable, messy, and full of moments that leave us wondering what direction to take next. You might feel like you’re doing all the “right” things and still end up unsure, overwhelmed, or disconnected from the life you imagined for yourself. That doesn’t mean you’ve failed. More often, it means you’re trying to steer without a compass.
That compass is your values.
Values are the guiding principles that help us choose how to move through the world. They give our days direction and our choices meaning. When we understand our values, we begin to understand ourselves not just who we are, but the kind of person we want to become.
If you read our previous article on living with intention you might remember the image of being in a boat without a paddle, just drifting wherever the current takes you. That metaphor still rings true here. When you know your values, you pick up the paddle. You steer. And what we’re unpacking now is how to know which way you want to steer, by clarifying your values, understanding the messages your emotions send, aligning goals behind what matters, and choosing to live more intentionally.
What Are Values?
Values are the qualities, ways of being, or themes that matter deeply to us. They aren’t rules or expectations, and they’re not about what other people say should be important. Think of them more like the wind that fills your sails. They help create a steady source of motivation and direction that helps you move toward a meaningful life.
Someone may value creativity, while another values reliability, play, compassion, or adventure. You might care deeply about curiosity in your work and connection in your closest relationships. None of these are right or wrong; they simply reflect what matters most to you.
Values are ongoing. You never “finish” kindness or integrity. They’re not tasks you check off a list, they’re qualities you practice, again and again. Goals can be completed; values stay with you, guiding how you show up each day.
Something that often gets missed in conversations about values is how personal they are. Two people can share the same value, yet define and live it in totally different ways. For example, someone who values connection may think of regular phone calls with loved ones, while another expresses that same value through hosting dinners, quality time, or simply being fully present during conversations. Neither is “more right” they’re just different interpretations of the same core value.
That’s why it’s so important to define your values in your own words. Without that clarity, it’s easy to get pulled into what you think a value “should” look like rather than staying true to what feels most authentic. When you understand what a value means to you, it becomes easier to notice when you’re living it, when you’ve drifted from it, and how you might lean into it more intentionally.
Why Values Can Feel Confusing
In my work with clients, I often hear people say they “know” their values. And in a broad sense, many do. They may identify with a long list of ideas such as honesty, family, creativity, balance, or achievement. However when we begin exploring more deeply, people are often unsure which values are their core values and which are simply qualities they feel they should care about.
This confusion makes a lot of sense. Most of us were never taught how to define our values, let alone how to organize them. When you look at a long list, it’s easy to assume all values should be equally important. But that belief can leave us overwhelmed and stuck.
We cannot actively embody all values all the time. It’s simply not possible. Trying to honor every value at once can create pressure rather than clarity. Instead of guiding us, values begin to feel like another task list we’re constantly failing to complete.
Clarifying which values are central in your life allows you to make choices with more ease. It doesn’t mean you ignore everything else; it just means you are choosing direction based on what is most important in this season of life. Naming a smaller set of core values allows you to move with intention rather than getting pulled in every direction at once.
How Emotions Help Us Understand Our Values
Our emotions can be some of the clearest signals of what matters to us, almost like a built-in notification system. When a feeling shows up (especially the uncomfortable ones), it’s often pointing toward a value that was touched, threatened, or honored.
Guilt is a common example. It doesn’t always mean you did something “wrong.” Sometimes guilt simply shows up when we’ve stepped away from something that feels important. If someone tells a lie and immediately feels unsettled, that reaction may be their internal signal that honesty is a value they want to live by.
Emotions can also show up when two values pull in different directions. Think about a moment where you’ve had to cancel plans with a friend because a family need came up. You honored your value around family, but guilt may still surface because dependability or commitment also matters to you. Both values are valid, your emotions are just reflecting the tension between them.
Even more subtle feelings can highlight what we care about. Sadness after a friend moves away can show how much connection matters. Frustration in an unfair situation can highlight a strong value around justice or respect. Anxiety may reveal a desire for stability, clarity, or safety.
Emotions aren’t always comfortable, but they’re meaningful. When we treat them as information instead of problems, they can help us identify which values are asking for attention and guide us back toward what feels aligned.
Finding Your Core Values
Knowing your values is one thing. Knowing which ones are your core values, the ones that truly guide your decisions and give your life direction, is another. Many people have a long list of values, however they often get stuck on how to narrow that list it down to the few values that really matter most.
A practical approach is to look for patterns in your choices over time.
When tough decisions arise:
-Which principles consistently guide you?
-Which values are non-negotiable?
These repeated priorities are usually your core values.
It’s also helpful to consider your motivations behind your goals and actions. Ask yourself: Why does this matter to me? If your answer connects to a deeper principle, that principle may be one of your core values.
Your core values are the ones that persist, even when life gets complicated.
Putting Values Into Action
Knowing your values is helpful, but the real change happens when you begin using them to guide how you live. This doesn’t have to involve sweeping life changes. Small steps can be incredibly meaningful.
Someone who values growth might begin trying new things, even if they feel unsure or awkward. A person who values connection might send a message to someone they care about. Someone who values health might begin prioritizing sleep or adding movement into their day. A person who values creativity might carve out a few minutes to write, paint, or build something.
In “Living With Intention,” we talked about small intentional choices such as pausing before a response, scheduling time for what matters, tidying a space to clear mental clutter. Those are exactly the kinds of acts that come alive when your values are clear. With your values guiding the way, you can select intentional actions that reflect them, making it easier to steer toward what matters rather than just reacting.
Living by your values is about nudging your life in the direction that matters to you, little by little, until those small actions add up.
A Values-Aligned Life Isn’t Always Easy
There’s a common misconception that once you know your values, everything suddenly becomes easy. In reality, living by your values can be uncomfortable.
Aligning with your values might mean saying no when you want to please others, setting boundaries, being honest when it feels vulnerable, or making choices others don’t understand. It can require sitting with discomfort, including doubt, frustration, embarrassment, or fear.
Life also gets busy. Stress piles up. Routines take over. Sometimes, disconnecting from what matters feels easier in the moment because we may simply not have the energy. So when you notice you’ve disconnected from your values, it’s important to recognize that this is normal and will happen at times.
Living a values-aligned life isn’t about perfection. It’s a practice. It’s about noticing when you drift and gently coming back.
Your Life, Guided by What Matters Most
Values help us make choices that feel meaningful and authentic, even when life feels messy. They help us notice what we care about and move toward it. Checking in with yourself regularly can be helpful:
-What mattered to you today?
-Did your choices reflect what’s important to you?
-What got in the way?
-And what small step could you take tomorrow?
Values aren’t about meeting some ideal version of yourself. They’re about being intentional. When you keep coming back to what matters most, you shape your life in a way that leads to fulfillment.
Understanding Neurodivergence and Masking: The Hidden Effort of Fitting In
Masking is a common yet often unseen experience for many neurodivergent individuals. It involves hiding or changing parts of oneself to fit in — a skill that can help in the short term but often leads to exhaustion and disconnection. This post explores what masking looks like, its emotional impact, and how caregivers and loved ones can support authenticity and self-acceptance.
Masking can feel like living with a dimmer switch turned down. Your true self is still shining underneath, just softened to fit in. For many neurodivergent people, including those with autism, ADHD, and other forms of neurodiversity, masking can serve as a short-term source of safety and belonging. Masking involves consciously or unconsciously hiding traits, stimming behaviors, or ways of thinking that might be perceived as unusual. It helps people navigate social expectations, avoid rejection, and protect against vulnerability in environments that may not yet feel accepting.
But while masking can be protective in the moment, it often comes at a cost. Over time, continually hiding parts of yourself can lead to emotional exhaustion, disconnection, and burnout. This blog explores what masking is, why it happens, and how caregivers and supports can help neurodivergent individuals feel safe turning their light back up.
What Masking Looks Like
Masking can take many forms, including:
Mimicking social behaviors such as making eye contact or mirroring gestures
Suppressing stimming behaviors like fidgeting or hand-flapping
Rehearsing conversations to appear more “typical”
Hiding challenges with attention, executive functioning, or sensory sensitivities
Why People Mask
Masking often arises from a desire to avoid judgment, bullying, or exclusion. From an early age, neurodivergent individuals may receive feedback that their natural behaviors are “wrong” or “awkward,” leading them to develop strategies to blend in. For some, masking can be a necessary coping mechanism, but for many, it becomes exhausting over time.
Why It’s Hard to Stop Masking
Even when people recognize how draining masking can be, it may feel uncomfortable or even scary to stop. Masking can become second nature after years of practice and self-protection. Many neurodivergent individuals worry about being misunderstood, rejected, or losing relationships if they begin showing more of their authentic selves.
Masking also serves an important short-term purpose. It can create a sense of safety by helping someone avoid vulnerability or emotional risk in environments that do not feel accepting. In moments where authenticity could invite criticism or harm, masking can be a protective shield that helps someone get through the day.
The challenge is that what starts as protection can become exhausting when used constantly. Over time, staying hidden can make it harder to feel seen, connected, and genuine. Unmasking takes time and gentleness. It is less about removing the mask completely and more about finding safe spaces where authenticity feels possible. Every step toward openness is an act of courage and self-trust.
What Masking Looks Like
Masking can take many forms, including:
• Mimicking social behaviors such as making eye contact or mirroring gestures
• Suppressing stimming behaviors like fidgeting or hand-flapping
• Rehearsing conversations to appear more “typical”
• Hiding challenges with attention, executive functioning, or sensory sensitivities
These are common examples of neurodivergent masking, often learned unconsciously over years of trying to adapt to expectations in school, work, or relationships.
Signs You Might Be Masking Without Realizing
Many neurodivergent people become so used to masking that it feels automatic. You might not even realize how often you’re doing it. Some common signs include:
• Feeling “on” or performative in social settings and exhausted afterward
• Replaying conversations or worrying about how you came across
• Adjusting your tone, expressions, or body language to match others
• Struggling to relax or act naturally around people outside your closest circle
• Needing long periods alone to recharge after social interactions
• Feeling unsure who you are when you’re not trying to fit in
Recognizing these patterns can be the first step toward greater self-awareness. Noticing when and where you mask can help you identify the environments that feel safe and those that require extra energy. Over time, creating neurodiversity-affirming spaces that welcome authenticity and celebrate individual differences can help reduce the need for masking and support long-term well-being.
The Cost of Masking
Consistently masking can contribute to stress, anxiety, depression, and burnout. The effort to constantly monitor and modify behavior can be mentally draining, leaving individuals feeling disconnected from their authentic selves. While masking can protect from vulnerability, it also serves as a barrier to allowing for genuine connection with others. If one is constantly masking around others, it prevents the opportunity for acceptance and authentic interactions. Many people only realize the extent of their masking later in life, often after experiencing prolonged stress or identity struggles.
Supporting Neurodivergent Individuals
Caregivers, teachers, and loved ones play a key role in noticing signs of masking. Some indicators include:
Appearing unusually tired or irritable after social interactions
Spending excessive time preparing for conversations or social situations
Experiencing physical symptoms of stress such as headaches or stomachaches
Withdrawing from activities they previously enjoyed
Acting very different in public than in private settings
Supports can help by creating safe environments where neurodivergent individuals feel comfortable expressing themselves without judgment. Encouraging small acts of authenticity, validating emotions, and offering accommodations can reduce the pressure to mask. Practical ways to do this include checking in about how social situations feel, modeling acceptance of differences, celebrating efforts to be authentic, and providing predictable routines or spaces where the individual can relax and be themselves.
Signs of Healthy Self-Expression
Healthy self-expression looks different for everyone, but may include:
Comfort in engaging in natural behaviors without shame or self-consciousness
Openly sharing thoughts, feelings, and interests with supportive people
Using coping strategies that feel sustainable rather than exhausting
Feeling a sense of relief or satisfaction after social interactions instead of burnout
The Role of Therapy in Unmasking
Therapy can be a powerful space for learning to unmask safely. A neurodiversity-affirming therapist helps clients explore the emotions tied to masking, rebuild a sense of self, and create strategies for authentic living that balance comfort and safety.
In therapy, individuals can process the stress and burnout that often accompany long-term masking. They can also practice setting boundaries, identifying triggers, and reconnecting with parts of themselves that were once hidden. Unmasking is a gradual process, and therapy offers a compassionate and safe environment for that growth.
Practical Tips for Reducing Masking
Individuals can take steps to reduce masking in daily life:
Practice small acts of authenticity, such as expressing a preference or opinion in safe settings
Create “mask-free” spaces at home, school, or work where authenticity is encouraged
Seek supportive communities where neurodivergent traits are accepted and valued
Set achievable goals for social interactions, gradually reducing the need to mask
Use mindfulness or self-affirmation to stay connected to personal feelings and needs
Embracing Neurodivergence
Awareness and acceptance of neurodivergence are crucial for reducing the pressure to mask. Environments that honor different ways of thinking, communicating, and interacting allow individuals to thrive without hiding who they are. Therapy, support groups, and advocacy can help neurodivergent individuals explore their authentic self, set boundaries, and practice self-compassion.
Moving Forward
If you notice yourself masking frequently, consider small steps toward authenticity:
Identify situations where masking is most intense
Allow yourself moments of natural behavior
Seek communities or relationships where you feel safe being yourself
Consider professional support to process the emotional impact of masking
Masking is a survival strategy, but it doesn’t have to define your life. For many neurodivergent individuals, masking has been a way to survive in a world that wasn’t built for them. Learning to unmask isn’t about flipping the lights on all at once, it’s about gently turning up the dimmer switch, one safe space and one act of authenticity at a time. With compassion, support, and self-acceptance, your true light can shine more freely, illuminating the best parts of you that’s always been there.
Why We Struggle with Communication (Even Though We Do It All the Time)
Even though we talk constantly, many of us struggle with effective communication. This blog explores the four main communication styles—passive, passive-aggressive, aggressive, and assertive—by walking through a conflict scenario and showing how each style plays out. It highlights the role of empathy, the importance of boundaries, and the balance between being direct and kind (drawing on DBT interpersonal effectiveness skills). It also discusses the limits of technology in conversations and why self-empathy matters just as much as empathy for others. Practical tools like a simple boundary-setting script, reflection questions, and exercises make the post actionable for readers who want to strengthen their relationships.
We talk every day, sometimes nonstop. Conversations with coworkers, friends, partners, family, even quick exchanges with strangers. Yet despite all this practice, many of us aren’t actually very good at communicating effectively. We stumble, misinterpret, over-explain, avoid, or escalate without realizing it. Good communication is a skill, not something that comes automatically.
Different Communication Styles
Most people lean into one of four main communication styles. Understanding them can help us notice our own patterns, and the patterns of others:
Passive – Avoids conflict at all costs, often staying silent even when feelings are hurt. Short-term peace, but long-term resentment builds.
Passive-Aggressive – Pretends everything is fine on the surface while expressing frustration indirectly (sarcasm, guilt-trips, the silent treatment). Creates confusion and mistrust.
Aggressive – Speaks loudly, forcefully, and sometimes disrespectfully. Gets the point across, but often damages relationships.
Assertive – Communicates directly, respectfully, and with clarity. Balances honesty with empathy. Assertive communication tends to lead to the healthiest and most sustainable outcomes.
One Conflict, Four Styles
Imagine this scenario: A friend cancels plans last minute, and your feelings are hurt. Here’s how the conversation might play out depending on your style—and how the other person may respond.
Passive
You: “It’s fine, don’t worry about it.”
Friend: Relieved and moves on, assuming you’re not upset. Meanwhile, your hurt feelings remain unspoken.
Passive-Aggressive
You: “Wow, must be nice to have so much free time to cancel on people.”
Friend: Feels confused or defensive. They may think, “Are they mad at me or joking?” The relationship tension lingers without clarity.
Aggressive
You: “You’re so unreliable! You clearly don’t care about me.”
Friend: Likely to become defensive or angry, firing back or shutting down. The focus shifts from your hurt to a bigger argument.
Assertive
You: “I felt hurt when you canceled at the last minute. I understand things come up, but I’d appreciate more notice next time.”
Friend: More likely to apologize and explain, without feeling attacked. This response leaves space for understanding, repair, and moving forward.
This highlights something important: the way we speak often shapes how the other person responds. Our tone and delivery can either open the door to connection or shut it down.
Empathy: The Core of Connection
Empathy isn’t just about being nice—it’s a skill set. Brené Brown describes four essential parts of empathy:
Perspective Taking – Seeing the situation from the other person’s viewpoint.
Staying Out of Judgment – Resisting the urge to criticize or evaluate their feelings.
Recognizing Emotion – Identifying what they’re experiencing.
Communicating Recognition – Letting them know they’ve been heard and understood.
Empathy is powerful because it says, “I’m willing to sit with you in this emotion without fixing, minimizing, or blaming.”
Why Empathy Feels Hard
Empathy requires vulnerability. To connect with someone’s sadness, fear, or frustration, we often have to touch those same emotions within ourselves. That’s uncomfortable, which is why we sometimes default to advice, distraction, or blame.
And here’s a common fear: “If I focus on their feelings, does that mean I’m dismissing mine?” But empathy doesn’t erase your needs. It simply acknowledges the other person’s emotional reality. The balance comes in pairing empathy with boundaries.
Boundaries: Empathy With Self-Respect
A healthy boundary is a way of saying, “I can care about how you feel, and I can still care about my own needs.”
For example:
Empathy without boundaries might sound like: “I understand you were stressed, so I’ll just let it go, even though I’m still hurt.” (Leads to resentment.)
A boundary with empathy might sound like: “I get that you had a lot going on. At the same time, I still felt hurt. I’d like us to find a better way to handle this next time.”
Boundaries are not walls. They’re guidelines for people around us to maintain healthy connections with us. When paired with empathy, they prevent burnout, resentment, and people-pleasing.
A Simple Script for Setting Boundaries
Boundaries don’t have to be complicated. A helpful framework is:
“When X (neutral event) happens, I feel Y (emotion), and I need Z (positive need).”
This structure keeps the focus on your feelings and needs rather than blame or criticism. It’s important to remember that we communicate our need in a way that is actionable for the other person. Often, we’re quick to focus on the negative behavior—what we don’t want—however when we do that, we lose sight of clearly communicating the behavior we do want to see moving forward.
Examples:
Friendship: “When plans get canceled last minute (X), I feel hurt and unimportant (Y). I need more notice if things change (Z).”
Work: “When meetings run late without warning (X), I feel stressed and overwhelmed (Y). I need to know in advance if we’ll go over time (Z).”
Family: “When my privacy isn’t respected (X), I feel frustrated (Y). I need some quiet time in the evenings to recharge (Z).”
Using this approach helps you stay assertive, empathetic, and clear—without over-explaining, drifting into aggression, or avoiding the conversation altogether. It centers your needs while giving the other person a clear path to respond positively.
The Blame Game
Brené Brown often describes blame as “a way to discharge discomfort and pain.” When something goes wrong, our minds want a target — someone or something to point to — because blame gives the illusion of control. It feels easier to say, “This is your fault,” than to sit with the discomfort of hurt, disappointment, or vulnerability.
But when we focus on blame, we step away from accountability and lose sight of what actually matters — our feelings and needs in the situation. Instead of identifying, “I felt hurt when that happened,” or “I needed to feel understood,” blame pushes us into defense mode.
Once blame enters the conversation, defensiveness quickly follows. The other person stops listening because they’re busy protecting themselves. We stop listening because we’re focused on being right. The conversation shifts from repair to combat, and the original issue — the hurt, misunderstanding, or unmet need — gets buried under a tug-of-war over who’s at fault.
Blame also keeps us from genuine self-reflection. It becomes the opposite of accountability:
Accountability says, “Here’s my part, and I’m willing to own it.”
Blame says, “This isn’t my fault, and I won’t change.”
The goal isn’t to avoid responsibility — it’s to stay curious and compassionate. Instead of, “Who’s to blame?” we can ask, “What happened here?” or “What was I feeling in that moment?”
This shift opens space for empathy and understanding, allowing both people to move toward resolution rather than staying trapped in reaction.
Why We Over-Explain (and Why Less Is More)
When we’re anxious about being misunderstood or fear disappointing someone, we often start over-explaining: adding more words, more context, and more apologies. Deep down, it’s usually an attempt to manage other people’s emotions or control how they perceive us.
But over-explaining often backfires. The more we talk, the more the message gets lost. Instead of clarity, we create confusion or defensiveness.
Over-explaining sounds like:
“I’m sorry, I didn’t mean it like that, I just thought maybe if you had time — but it’s totally fine if you don’t!”
It can come from a place of people-pleasing or fear of rejection. We hope that by softening or over-qualifying our message, we’ll avoid conflict. But in reality, it dilutes our needs and boundaries.
Less is more. A clear, calm statement is more likely to be heard than a long, anxious one.
Try this shift:
Instead of: “I’m sorry, I know you’re busy, but it just kind of hurt when you didn’t reply. I totally get it though, I know you have a lot going on.”
Say: “I felt hurt when I didn’t hear back. Is everything okay between us?”
Directness feels uncomfortable at first because it is more vulnerable, however it communicates self-respect and empathy in two sentences.
Technology: A Blessing and a Barrier
Technology makes staying connected easier than ever. A quick text can confirm plans, check in on a loved one, or share encouragement in seconds. Video calls allow us to see the faces of friends and family across the world. Social media keeps us updated on people’s lives even when distance separates us.
But there’s a downside: over-reliance on technology can weaken real communication. Tone gets lost in text. Emojis and punctuation can be misread. Silence can feel like rejection. And sometimes, hiding behind a screen feels safer than having a vulnerable, honest conversation face-to-face.
Another risk is that relationships can get stuck at a surface level. It’s easy to “like” a post, send an emoji, or fire off a quick text—but those interactions don’t always deepen trust or understanding. They give the appearance of connection without the substance. True connection often requires slowing down, listening, and being present with someone’s full emotional experience—something much harder to capture in a short digital exchange.
Technology works best as a support, not a replacement. It’s great for convenience, but meaningful conversations often need more—our voices, facial expressions, and presence. Sometimes the best way to resolve conflict or express care is still the old-fashioned way: talking in person or picking up the phone.
Start With Self-Empathy
One piece often overlooked: how we talk to ourselves. If your inner dialogue is harsh—“I’m stupid, I always mess this up”—it’s harder to speak kindly and assertively with others. The way we communicate externally often mirrors the way we communicate internally.
Self-empathy means extending the same compassion and understanding towards yourself that you’d naturally offer a friend. Instead of criticizing yourself for mistakes, you pause to acknowledge your feelings with curiosity and care.
Recognize what you feel – “I’m anxious right now.”
Validate the emotion – “It makes sense I feel this way after that conversation.”
Offer kindness instead of judgment – “I’m learning, and it’s okay not to have this perfect.”
Something important to emphasize here is that self-empathy is not self-pity. It doesn’t mean excusing harmful choices or avoiding accountability. Instead, it provides the emotional safety net that allows you to grow and change without shame.
And just like with others, self-empathy pairs best with boundaries. You can be gentle with yourself and hold yourself accountable:
“I didn’t communicate clearly this time. That doesn’t make me a failure, and I’ll practice being more direct next time.”
When we strengthen our capacity for self-empathy, we become less reactive and more grounded. That steadiness makes it easier to communicate with others in a way that is both compassionate and assertive.
Try This: A Quick Skill-Building Practice
You don’t need a big workbook to start practicing—just a few intentional steps can make a big difference.
Think of a recent conflict or miscommunication.
Write out what you actually said.
Then rewrite it in an assertive + empathetic format, using the “When X, I feel Y, I need Z” script.
Optional: practice saying it out loud in front of a mirror.
This simple exercise can help build confidence in communicating more clearly and effectively. After practicing, notice how the conversation feels. Did you come across clearer? Did the other person respond differently? Communication is a skill, and progress comes from reflection and repetition, not perfection.
Takeaway
We all talk, but talking isn’t the same as communicating effectively. Becoming aware of your communication style, practicing empathy (for yourself and others), setting boundaries, and leaning into clear, assertive expression can strengthen your relationships.
And remember: the way you communicate shapes how the other person responds. Blame builds walls. Empathy builds bridges. Boundaries keep the bridge safe and sturdy. Say less when you can, listen more, and keep it genuine.
Reflection Questions
Which communication style do I use most often—passive, passive-aggressive, aggressive, or assertive?
How does my communication style influence how others respond to me?
When was the last time empathy helped me connect with someone?
Where might I need to pair empathy with stronger boundaries?
How do I speak to myself—and how does that affect how I speak to others?
OCD vs. Anxiety: Why the Difference Matters
OCD is often mistaken for generalized anxiety, which can lead to misdiagnosis and treatment that doesn’t fully address the root problem. This blog explores the key differences between OCD and anxiety, highlights how OCD symptoms can show up in less visible ways (like Pure O and internal compulsions), and explains why recognizing OCD subtypes matters—even though they aren’t formally listed in the DSM-5. We also discuss treatment options beyond ERP, including CBT, ACT, and medication, while offering practical tips for loved ones to support someone with OCD without falling into reassurance cycles.
Alex had been struggling for years with constant worry that he wasn’t being productive enough. He would spend hours mentally reviewing tasks, repeatedly checking his work, and feeling tense and anxious. He sought treatment for anxiety, but while therapy helped him manage some stress, the underlying distress didn’t go away. What was missing? Alex actually had OCD, and his intrusive thoughts and mental rituals required specialized treatment.
Many people like Alex are misdiagnosed because OCD symptoms, such as repetitive worries, intrusive thoughts, or mental checking, can look a lot like generalized anxiety. This can lead to treatments that address only the surface anxiety, leaving the obsessive-compulsive cycle intact. Understanding the difference between OCD and anxiety is crucial to getting the right care and support.
The Scope and Impact of OCD
OCD is more common than many realize, affecting about 2–3% of the population worldwide. Unfortunately, research shows it can take an average of 7–10 years from the onset of symptoms for someone to receive the correct diagnosis and treatment. In that time, OCD can interfere with school, work, relationships, and quality of life.
Why OCD Is Often Missed as a Diagnosis
OCD and anxiety share many similarities. Both involve intense worry, fear, and physical symptoms like restlessness or racing thoughts. What makes OCD different is the presence of obsessions (intrusive, unwanted thoughts or images) and compulsions (behaviors or mental rituals done to reduce distress).
Because the anxiety caused by OCD is so strong, many people (and even clinicians) may focus only on the anxiety symptoms, overlooking the underlying obsessive-compulsive cycle. This can lead to a diagnosis of “generalized anxiety” without recognizing that the core issue is OCD. Missing the diagnosis often delays access to the specific treatments.
The Shame and Stigma Factor
One of the biggest reasons OCD goes unnoticed is shame. People often fear judgment for their intrusive thoughts—especially when those thoughts are violent, sexual, or go against their values. Misunderstandings like “we’re all a little OCD” trivialize the condition, making it harder for people to open up. The secrecy fueled by shame delays help, allowing symptoms to grow stronger over time.
Breaking this stigma is critical. Talking openly about the wide range of OCD presentations helps normalize the experience and reminds people that intrusive thoughts do not reflect character or intent.
A Closer Look: OCD vs. Anxiety in Action
To understand the difference, let’s compare two scenarios:
Anxiety example: Someone may worry about forgetting to lock the door before leaving for work. They might briefly double-check, then go about their day still carrying some unease.
OCD example: Someone with OCD may feel overwhelmed by an intrusive fear that if they don’t lock the door just right, something terrible will happen. To quiet the distress, they may check the lock dozens of times, replay memories to “make sure,” or even avoid leaving home altogether.
Both involve worry, but OCD creates a cycle of obsessions and compulsions that can consume hours of the day and significantly disrupt life.
Subtypes of OCD and Why They Matter
Even though the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders) doesn’t officially break OCD into categories, many clinicians and people with lived experience talk about different “subtypes.” You might hear that there are around 18 themes, like contamination, checking, harm, scrupulosity, relationship OCD, or Pure O.
The reason the DSM-5 doesn’t separate them is because the underlying cycle of OCD (obsessions leading to compulsions) is the same no matter the theme. Whether someone is washing their hands dozens of times or replaying a thought in their mind, the brain process is similar.
Still, talking about subtypes can be really useful. It helps people realize they’re not alone or “weird” for the kinds of thoughts they have, and it gives language to something that often feels isolating. It also helps therapists shape treatment in a way that fits.
So while subtypes aren’t official in the diagnostic manual, they’re still important to recognize. They make the experience of OCD more understandable, and they remind people that their symptoms are valid.
More Recognized Subtypes of OCD
OCD doesn’t look the same for everyone. Subtypes describe common themes obsessions and compulsions may take, but it’s important to remember that OCD can attach itself to almost any area of life. Here are some of the more recognized subtypes:
Contamination OCD: Intense fears of germs, illness, or unclean environments. Compulsions often include excessive washing, cleaning, or avoiding certain places or people.
Checking OCD: Repeatedly checking things—locks, appliances, emails, or even memories—to relieve fears of causing harm or making a mistake.
Harm OCD: Intrusive thoughts of accidentally or intentionally hurting oneself or others. These thoughts are distressing and unwanted, often leading to avoidance or mental rituals for reassurance.
Religious or Scrupulosity OCD: Obsessions centered on morality, blasphemy, or offending a higher power. Compulsions might include excessive praying, confession, or seeking reassurance about being “good enough.”
Sexual or Relationship OCD: Disturbing intrusive thoughts about sexuality, fidelity, or attraction. Compulsions may involve seeking reassurance, avoiding intimacy, or mentally analyzing feelings.
Symmetry and Ordering OCD: A need for things to feel “just right.” This might involve arranging objects symmetrically or repeating actions until they feel correct.
Sensorimotor (Somatic) OCD: Persistent awareness of automatic bodily functions such as breathing that can lead to hypervigilance
What About “Pure O”?
Another term that often comes up is Pure O, short for “purely obsessional OCD.” Many people with OCD describe experiencing only obsessions—distressing intrusive thoughts, images, or doubts—without the visible, outward compulsions like handwashing or checking.
It’s important to note, however, that Pure O doesn’t mean there are no compulsions at all. Instead, the compulsions are often internal or mental, making them harder to spot. For example, someone may silently repeat phrases, pray, review past events for reassurance, or mentally check whether they felt the “right” emotion. These hidden rituals provide temporary relief but keep the OCD cycle going.
Because these compulsions aren’t obvious, Pure O is especially likely to be mistaken for anxiety or rumination. This makes awareness crucial: intrusive thoughts alone don’t define OCD. It’s the cycle of obsessions and compulsions, whether visible or invisible, that makes it OCD.
OCD as a Spectrum
Another key point is that OCD exists on a spectrum. Someone may primarily struggle with one theme, such as contamination fears, but later develop obsessions in a completely different area, such as relationships or morality. Shifts in themes over time are common, and many people live with multiple subtypes at once. Recognizing OCD as a spectrum helps us understand that it isn’t limited to one “look” or set of behaviors.
For Loved Ones: How to Support Someone with OCD
Supporting a loved one with OCD can feel confusing—you want to ease their distress, but sometimes reassurance or accommodation can unintentionally reinforce the OCD cycle. Here are some ways to show care without fueling symptoms:
Educate Yourself: Learning the basics of OCD helps you separate your loved one’s values and personality from the intrusive thoughts they struggle with. OCD is not a choice, and the compulsions are driven by real distress.
Offer Compassion, Not Reassurance: Constant reassurance (“You’re fine, you did enough today”) can actually strengthen OCD’s grip, because it trains the brain to rely on others for temporary relief. Instead, try validating the feeling without confirming or denying the worry:
Instead of: “Don’t worry, you were really productive today.”
Try: “I can see how stressful those thoughts about productivity feel. I believe you’re working hard on handling them.”
Set Healthy Boundaries: Boundaries aren’t about withholding love—they’re about creating balance and protecting both people’s well-being. Examples might include:
“I care about you, but I can’t keep checking your to-do list every night. I’ll cheer you on while you practice trusting yourself instead.”
“I won’t be able to answer the same productivity question over and over, but I’m happy to sit with you while you ride out the anxiety.”
“I love you, and I want to support your therapy homework instead of doing the rituals for you.”
Encourage Professional Help: ERP is considered the gold standard for OCD treatment, but it’s not the only approach. Cognitive Behavioral Therapy (CBT), Acceptance and Commitment Therapy (ACT), and medication can also be part of effective treatment. Sometimes a combination provides the best outcome.
Support Progress, Not Perfection: Recovery from OCD isn’t linear. There will be setbacks, and that’s normal. Offer encouragement when your loved one tries something hard, rather than focusing only on the outcome.
Important Reminder: You don’t have to become your loved one’s therapist. Your role is to provide steady support, encouragement, and boundaries that honor both their recovery journey and your own well-being.
Closing Thoughts
OCD can be overwhelming, isolating, and misunderstood—but it is also highly treatable. Recognizing the difference between anxiety and OCD is a powerful first step toward the right kind of help. With evidence-based therapies, support from loved ones, and compassion for the journey, recovery is possible.
If you’re supporting someone with OCD, remember: you don’t need all the answers. What matters most is patience, empathy, and setting boundaries that protect both of you. And if you’re the one living with OCD, know that your intrusive thoughts are not a reflection of who you are, they are a symptom of a disorder that you can learn to manage.
There is hope, and there are tools. While healing doesn’t mean eliminating every intrusive thought. Healing does mean learning to live fully without letting OCD call the shots. You are not alone, and with the right help, you can start connecting back to things that matter to you in life.
References & Resources
International OCD Foundation (IOCDF): https://iocdf.org
Offers education, research updates, and a provider directory for specialized OCD treatment.National Institute of Mental Health (NIMH): https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd
Provides an overview of OCD, symptoms, and treatment options.Anxiety & Depression Association of America (ADAA): https://adaa.org
Includes resources on OCD, anxiety, and evidence-based treatment approaches.Books:
Freedom from Obsessive-Compulsive Disorder by Jonathan Grayson, PhD
The Mindfulness Workbook for OCD by Jon Hershfield, MFT, & Tom Corboy, MFT
Overcoming Unwanted Intrusive Thoughts by Sally Winston, PsyD, & Martin Seif, PhD
OCD Unlocked: A Teen’s Workbook for Understanding and Thriving with OCD by Lillian Carlyle
The OCD Breakthrough Series (3 books) | by Cross Border Books
If you or someone you love is struggling, reaching out to a licensed mental health professional trained in OCD treatment is an important first step.
The Stages of Change: Why We Struggle to Follow Through (and How to Keep Moving Forward)
Change isn’t a straight line—it’s a process. The stages of change model reminds us that we move through phases like contemplation, planning, action, and maintenance, with the possibility of setbacks at any stage. Using the Passengers on the Bus metaphor from ACT, this blog explores why it’s so easy to slip back into old routines (like skipping the gym or abandoning new habits) and how values can guide us toward long-term change. Whether you’re working on your own growth or supporting someone else, understanding the stages of change helps us meet ourselves—and others—with more compassion and direction.
January rolls around, and suddenly the gym is packed. By March, the parking lot is empty again. Most of us know this pattern well. We set out with good intentions—going to the gym, eating better, saving money, or cutting back on social media—but the excitement fades, life gets in the way, and we slip back into old habits.
It’s not because we’re lazy or incapable. It’s because change isn’t a one-time decision—it’s a cycle. And understanding that cycle helps us stick with what matters and extend compassion to ourselves (and others) when we stumble.
The Five Stages of Change
1. Precontemplation – Not Yet Considering Change
Here, the idea of change isn’t even on our radar. Maybe we’ve thought, “I should probably exercise more,” but it doesn’t feel urgent or realistic.
Example: The gym shoes are buried in the closet. Friends invite you to join them for a class, but you shake your head—you’re not there yet.
2. Contemplation – Weighing Pros and Cons
This is the “thinking about it” stage. You know change might be helpful, but the barriers feel heavy.
“I’d feel healthier if I worked out… but I’m exhausted after work.”
“I want to save money… but online shopping is so easy.”
It’s common to stay here a while. Ambivalence is part of the process, not a flaw.
3. Preparation (Planning) – Setting Intentions
At this stage, we begin taking small steps: signing up for a gym membership, downloading a budgeting app, or putting our phone in another room before bed. We’re building readiness, but we haven’t built consistency yet.
The challenge? Sometimes planning feels like progress, and we mistake preparation for action.
4. Action – Doing the Thing
This is when change starts to happen. You’re going to the gym, tracking your spending, or sticking with a nighttime routine. Momentum builds—but so does resistance.
You might feel the pull of excuses, old patterns, or passengers on the bus (we’ll get to that in a moment). Motivation can spark the action stage, but habits keep it alive.
5. Maintenance – Stabilizing the Habit
Here, the change feels more natural. The gym is a regular part of your week. Saving money has become a rhythm. Screen time is more intentional.
Relapse
Relapse—sliding back into old patterns—can happen at any stage. A stressful week, travel, or illness might derail progress. It is important to normalize that relapse isn’t failure. It’s just part of the cycle.
Think about what it takes to build a new car. No company would release the very first prototype and expect it to be perfect. Engineers test, adjust, and rework the design over and over until it’s safe, reliable, and road-ready.
Change works the same way. Your first attempt at a new habit—whether it’s exercising, budgeting, or setting boundaries—probably won’t be flawless. You might stall, take a detour, or even go back to old patterns for a while. That doesn’t mean the change “failed.” It just means you’re still refining the model.
Relapse isn’t the end of the journey—it’s part of the testing process. Each time you return to the drawing board, you’re learning what works and what doesn’t, making it more likely that your “final version” will actually last.
Why We Lose Momentum
So why do we start strong and then stall?
Vague goals: “I’ll eat healthier” is hard to measure or sustain.
Loss of motivation: The spark fades, and life feels too busy.
Expectations about speed: We hope new habits stick in weeks, but research suggests it can take 2–12 months before a behavior feels automatic.
Discomfort: If change was easy, we would just do it. Real change is uncomfortable physically, emotionally or both. Change means we have to be okay with stepping outside our comfort zone and staying there for a while.
All-or-nothing thinking – Missing one workout, overspending once, or slipping up with a boundary doesn’t mean you’ve failed. But if we believe a misstep equals failure, we’re more likely to give up altogether.
This is why patience—and seeing ourselves through the stages of change—really matters. Building lasting change isn’t about speed; it’s about endurance. Think of it less like a sprint and more like training for a marathon. Setbacks are part of the process. What counts most isn’t whether you stumble, but how you respond: noticing when you’ve veered off course, choosing to regroup, and gently steering yourself back toward your values.
The Passengers on the Bus
A metaphor I often share is called Passengers on the Bus, from Acceptance and Commitment Therapy (ACT).
Imagine you’re the driver of a bus, following a familiar route. This route represents our daily routines—wake up, go to work, come home, go to sleep, repeat. Ideally, we want our bus to head in the direction of our values—things like health, balance, freedom, or connection. But sometimes, we realize that parts of our route no longer serve us, that is starting to disconnect us from our goals and values and that’s when we start thinking about change.
The passengers on the bus are your thoughts, feelings, and habits. They shout things like:
“You’re too tired today.”
“You’ll never stick with this.”
“It’s easier to do what you’ve always done.”
Often, we let these passengers steer us back onto the old, familiar route. It feels safe because we’ve driven it so many times before—we know the shortcuts, the potholes, ways to avoid the detours. But that comfort doesn’t mean it takes us where we want to go.
The goal isn’t to kick the passengers off (you can’t). The goal is to stay in the driver’s seat and keep steering toward what matters, even with their noise in the background. Your values are the compass that remind you why the route is worth it.
Practical Tips for Each Stage
Precontemplation: Focus on curiosity, not pressure. Ask yourself, “What might be different if I did make a change?”
Contemplation: Write out your pros and cons. Notice how your reasons for change connect with your values.
Preparation: Get specific. Not “exercise more,” but “walk 20 minutes after dinner three times a week.”
Action: Pair new habits with existing routines (change clothes after work, head straight to the gym). Build accountability—share your goal with a friend.
Maintenance: Create supports for the long haul. Celebrate milestones and track progress. Expect setbacks and have a plan to restart gently.
Relapse: Ask, “What pulled me off track? What small step will get me back on?” Think adjustment, not starting over.
Why Knowing the Stages Matters
Understanding your own stage helps you set realistic expectations and show yourself compassion when things don’t go perfectly. Knowing what stage you are in allows for you to:
Reduce shame – If you’re still in contemplation but expect yourself to be in action, you’ll feel like you’re failing. Recognizing your actual stage normalizes why you might not be ready to take big steps yet.
Match strategies to readiness – Different stages need different approaches. Someone in planning benefits from setting specific goals, while someone in precontemplation needs reflection and awareness first.
Build patience – Change isn’t just about “trying harder.” By seeing it as a process, you understand that setbacks are expected, not proof that you can’t change.
Help us support others – Knowing the stages also helps us meet friends, clients, or loved ones where they are, instead of pushing them ahead too quickly.
In short, knowing your stage gives you a map. Without that map, it’s easy to get lost in self-criticism or use strategies that don’t fit. With it, you can walk the path of change step by step, with more clarity and self-compassion.
Why This Matters for Supporting Others
Change is deeply personal, but it doesn’t happen in isolation. Recognizing the stages of change also helps us understand where others are. If a loved one isn’t ready for action, pushing harder won’t help—it can actually make them dig in more. This perspective can help reduce our frustration when someone isn’t “changing fast enough” and helps us set realistic expectations for their progress. Meeting people where they are, with empathy, makes change safer, more possible and allows us to stay healthy supports without burning ourselves out.
Final Takeaway
Change is rarely a straight line—it’s a cycle of progress, setbacks, and learning. By understanding the stages of change, we can meet ourselves (and others) with more patience, realistic expectations, and compassion. Whether you’re in contemplation, action, or somewhere in between, every step matters because it brings you closer to living in alignment with your values.
To take this from theory into practice, here are a few questions to reflect on:
Which stage of change am I in right now for the goal I’m working on?
What values matter most to me, and how does this goal connect with them?
What “passengers on the bus” (thoughts, feelings, or habits) tend to pull me back to the old route?
When I’ve relapsed in the past, what patterns or triggers showed up? What can I learn from them?
What’s one small, specific step I could take this week to move from my current stage toward the next?
If I’m supporting someone else, how can recognizing their stage reduce my frustration and help me set more realistic expectations for their progress?
What would self-compassion look like as I move through these stages?
Remember: the goal isn’t perfection—it’s persistence. Each loop through the cycle builds resilience, wisdom, and strength. Stay in the driver’s seat, keep your values as your compass, and allow yourself to keep moving toward what matters most.
Supporting a Loved One With an Eating Disorder
Supporting someone with an eating disorder (ED) can feel overwhelming, but your love, patience, and presence are powerful tools in their recovery. Eating disorders are serious mental health conditions—not a choice—and often serve as maladaptive coping mechanisms. They can be isolating, and recovery may uncover underlying struggles like anxiety, trauma, or depression.
When someone you love is struggling with an eating disorder, it can be painful to watch. You may feel helpless, unsure of what to say, or afraid of making things worse. Your presence, patience, and compassion are incredibly powerful. While eating disorders are complex mental health conditions that require professional support, loved ones play an essential role in the recovery journey.
Understanding Eating Disorders
Eating disorders affect nearly 30 million Americans at some point in their lifetime. They are not just about food or appearance—they are serious mental health conditions influenced by genetics, environment, trauma, and cultural pressures. Eating disorders have the second highest mortality rate of any mental health disorder (after opioid use disorder).
It’s also important to distinguish between disordered eating and a clinically diagnosed eating disorder. Disordered eating may include behaviors like skipping meals, chronic dieting, or rigid food rules, however an eating disorder typically involves more severe and persistent patterns that interfere with daily life, relationships, and health. Both deserve compassion and can benefit from support, and a diagnosed eating disorder often requires specialized treatment.
Eating disorders can also feel incredibly isolating. Many people withdraw from friends, family, and activities they once enjoyed. Reminding your loved one that they are valued beyond their illness—and that they don’t have to go through this alone—can help bridge that isolation.
Warning Signs to Look Out For
It can sometimes be hard to recognize when someone is struggling. Remember eating disorders are isolating and secretive by nature. A few potential red flags include:
Skipping meals or making excuses not to eat
Dramatic changes in weight (up or down)
Preoccupation with calories, weight, or body size
Avoiding social situations involving food
Excessive exercise or distress when exercise is interrupted
Rigid food rules (e.g., labeling foods “good” or “bad”)
Withdrawal from friends or activities
Extreme perfectionism or heightened anxiety around eating
Not every sign points to an eating disorder, but noticing patterns can help you gently open conversations and encourage professional support.
Myths & Misconceptions About Eating Disorders
Despite growing awareness, many misconceptions about eating disorders remain. Clearing them up is an important step toward reducing stigma and offering compassionate support.
Myth: Eating disorders are a choice.
Reality: No one would choose the pain, medical risks, and isolation that come with an eating disorder. They are serious mental health conditions—not diets gone too far or vanity projects.
Myth: Eating disorders are just about food or wanting to be thin.
Reality: Eating disorders often start out as maladaptive coping mechanisms—ways of managing overwhelming emotions, trauma, or stress. Food and body image become the focus, but underneath, the disorder may be helping someone feel in control, numb, or distracted from deeper pain.
Myth: Once someone stops the behaviors, they’re “better.”
Reality: Recovery involves peeling back the eating disorder behaviors, but when those are stripped away, underlying issues like anxiety, depression, or trauma often come forward. This is why professional treatment and ongoing support are so essential.
Myth: Only young, thin, white women struggle with eating disorders.
Reality: Eating disorders affect people of all genders, ages, races, body sizes, and backgrounds. Weight stigma and cultural bias often prevent people in larger bodies, men, or people of color from being recognized and treated.
Why Early Intervention Matters
The earlier someone receives support, the better the chances for full recovery. Waiting until “things get worse” can allow the disorder to become more entrenched. Even if you’re unsure whether your loved one’s behaviors are “serious enough,” it’s better to seek help sooner rather than later.
Medical Risks to Be Aware Of
Eating disorders can affect nearly every system in the body, including:
Heart health (arrhythmias, cardiac arrest)
Bone density (osteopenia, osteoporosis)
Fertility and hormones (menstrual changes, low testosterone)
Digestive health (slow motility, bloating, reflux)
Brain health (difficulty concentrating, mood instability)
These risks highlight why eating disorders need specialized medical and mental health care—not just willpower or lifestyle changes.
Treatment and the Team Approach
Effective treatment often involves a multidisciplinary team, ideally with each member specializing in eating disorders. A well-rounded team may include:
Therapist – using approaches like CBT-E, DBT, ACT, FBT, or trauma-informed therapy
Dietitian – trained in eating disorders, weight-inclusive care, and nutrition therapy
Physician or pediatrician – monitoring medical stability and complications
Psychiatrist – addressing co-occurring mental health conditions and medication needs
Why specialization matters: Not all providers are trained in eating disorders. Working with professionals who don’t specialize can sometimes be damaging—for example, if a provider emphasizes weight loss, uses diet culture language, or overlooks serious medical risks. A specialized team is better equipped to treat the whole person, not just the behaviors.
Having a professional treatment team also allows you to remain in the role of loved one—not dietitian or therapist role. This matters because sometimes the eating disorder resists or even lashes out against support. By trusting the professionals to guide treatment, you can focus on being a consistent, compassionate presence in your loved one’s life.
How You Can Help
1. Lead with compassion, not criticism
It can be tempting to reassure with comments about weight or eating (“you look healthy,” “just eat more”), but these often backfire. Instead, focus on expressing care:
“I love you and I’m here to support you.”
“I may not fully understand, but I want to be here for you.”
When commenting on appearance, shift the focus from body size to mood or energy:
Instead of “You look great,” try “You look really happy today.”
Instead of “You’ve lost/gained weight,” try “It’s so nice to see you enjoying yourself.”
2. Separate the person from the eating disorder
Your loved one is not their illness. It can help to think of the eating disorder as an external force that is influencing them, rather than who they are at their core. This perspective allows you to direct frustration toward the disorder, not your loved one, and remind them of their strengths outside of food, weight, or body image.
3. Think about your own language around food and body image
Comments like “I feel so fat” or “I need to burn this off” may seem harmless but can reinforce harmful thought patterns. Try to model neutral or positive language around food and body image. Celebrate what bodies can do rather than how they look, and talk about food as nourishment rather than something to earn or restrict.
4. Listen more than you speak
You don’t need to have the “right” words. Often, simply listening with openness and compassion is more healing than offering advice. Focus on creating a safe space where your loved one can share what feels comfortable. Show empathy by validating their feelings while still separating them from the eating disorder.
Example: Instead of saying “Just eat, you’ll feel better,” you might say, “I know eating feels really hard right now. Let me know how to support you.”
5. Do’s and Don’ts for Loved Ones
6. Educate yourself
Understanding the medical and emotional complexities of eating disorders can help you respond with empathy. Additionally, understanding systemic barriers to care is important. LGBTQ+ folks, BIPOC individuals, and those in larger bodies often face unique stigma and discrimination in accessing treatment. Pointing your loved one toward affirming, inclusive resources can make a difference. These resources can guide you:
National Eating Disorders Association (NEDA) – nationaleatingdisorders.org
National Alliance for Eating Disorders – allianceforeatingdisorders.com
The Trevor Project (for LGBTQ+ youth) – thetrevorproject.org
Health at Every Size (HAES) – Association for Size Diversity and Health
Books like Health at Every Size by Lindo Bacon, PhD, and Body Respect by Lindo Bacon & Lucy Aphramor
HAES promotes dignity, respect, and access to care for people of all body sizes. This framework helps challenge diet culture and weight stigma—two powerful risk factors that can fuel eating disorders.
7. Encourage professional help—gently
Eating disorders rarely resolve on their own. You can encourage your loved one to reach out for professional care, but avoid ultimatums. Sometimes offering to help research providers or go with them to an appointment can lower barriers.
8. Support daily life in practical ways
Eating disorders can make everyday situations (meals, social events, even doctor’s visits) overwhelming. Offering to sit with them during meals, provide distractions, or just be a grounding presence can help reduce isolation.
9. Take care of yourself, too
It’s common for caregivers to feel exhausted or even burnt out. Seeking your own support—whether therapy, a support group, or leaning on friends—allows you to keep showing up in a sustainable way.
10. Remember that recovery is not linear
Relapses and lapses can happen. Try not to see them as failures, but as part of the recovery process. Acknowledge the effort your loved one is putting in and celebrate even small steps forward.
When Your Loved One Isn’t Ready to Challenge Their Eating Disorder
It’s common for someone struggling with an eating disorder to feel ambivalent about recovery. As mentioned earlier, the eating disorder often serves as a maladaptive coping mechanism, offering a sense of control or comfort in the short term, while causing long term pain and suffering. Because of this, your loved one may not yet be ready or willing to challenge it.
As a caregiver, this can be incredibly difficult. You may feel helpless or frustrated when progress doesn’t come as quickly as you hope. In these moments, it’s important to remember: Recovery is not about forcing change. It’s about supporting readiness for change.
Here are a few things you can do:
Stay consistent with your care. Continue to show up with love, patience, and empathy—even if they reject support.
Set gentle boundaries. Supporting them doesn’t mean sacrificing your own well-being. It’s okay to say what you can and cannot do.
Focus on connection. Spend time together in ways unrelated to food or body image—watch a movie, go for a walk, or talk about something they enjoy.
Recovery is often a long, non-linear journey. Your role is not to fix the eating disorder. Your role is to provide steady love and support while the treatment team guides the clinical work.
Signs Your Loved One May Be Moving Toward Readiness
Even if your loved one isn’t actively challenging their eating disorder yet, you may notice small shifts that signal they’re beginning to consider recovery. These signs can be subtle but meaningful:
More openness in conversation. They start sharing thoughts or fears about food, body image, or recovery, even in small ways.
Less secrecy. You notice they’re slightly more transparent about behaviors or emotions.
Expressing ambivalence. They might say things like, “Part of me wants to get better, but I’m scared.” This shows they’re wrestling with the idea of change.
Willingness. They show curiosity about treatment options, coping skills, or stories of recovery.
Engagement in relationships. They begin reconnecting with people or activities outside of the eating disorder.
These steps may feel small, however they are signs that your loved one is beginning to imagine life beyond the eating disorder. Your role is to encourage these openings gently, without pushing too hard.
Caregiver Self-Checklist
Here are a few quick reminders to keep in mind as you support your loved one:
Lead with love and care — remind them they’re more than their eating disorder.
Watch your language — avoid diet talk, food shaming, or body comments.
Listen first — you don’t need to have all the answers.
Encourage, don’t pressure — offer support for professional help.
Care for yourself too — your well-being matters in this process.
Learn weight-inclusive approaches — explore HAES to challenge harmful diet culture messages.
Final Thoughts
Supporting a loved one with an eating disorder doesn’t mean fixing it—that’s not your responsibility. What you can do is show up with love, patience, and consistency. Your support, combined with professional treatment, can be a lifeline.
If you or your loved one need immediate support, you can call or text the 988 Suicide & Crisis Lifeline, or reach out to the NEDA Helpline at (800) 931-2237 for guidance.
Recovery is possible, and your loved one is so much more than their eating disorder.
Life After Birth: Navigating Postpartum Mental Health and Identity
Motherhood is a beautiful, transformative experience—but it also comes with emotional, physical, and identity challenges. Postpartum depression and anxiety are more common than many realize, affecting about 1 in 5 new parents. This blog explores the signs and symptoms of postpartum mood disorders, the adjustment to life with a newborn, the healing of your body, and shifts in self-identity.
Becoming a parent is often described as one of life’s most joyful experiences—and for many, the postpartum period brings unexpected challenges alongside the love and wonder of meeting a new baby. Speaking from my own recent experience, I remember eagerly anticipating meeting my baby (and, honestly, not being pregnant anymore!)—only to dive into the enormous life shift of navigating daily life with a newborn, putting aside work and other routines, and fully embracing the role of motherhood.
It’s a season of transition, and with transition often comes stress, uncertainty, and vulnerability. If you’ve found yourself feeling both grateful and overwhelmed, you are not alone. In fact, research shows that about 1 in 5 women experience postpartum depression or anxiety, making these struggles far more common than many realize.
Postpartum Depression and Anxiety: Signs to Notice
Some emotional ups and downs are common after birth, often called the “baby blues.” But postpartum depression (PPD) and postpartum anxiety (PPA) go beyond that—they are heavier, longer-lasting, and can interfere with daily life.
Signs of postpartum depression may include:
Persistent sadness, emptiness, or hopelessness
Feeling disconnected from your baby or struggling to bond
Loss of interest in activities you once enjoyed
Changes in appetite or sleep (beyond newborn-related changes)
Intense feelings of guilt, shame, or worthlessness
Signs of postpartum anxiety may include:
Constant worry, often about your baby’s safety or your ability to parent
Racing thoughts that won’t quiet down
Physical tension—like a racing heart or difficulty breathing
Trouble sleeping even when the baby sleeps
Intrusive thoughts that feel scary or hard to control
While postpartum depression has become more widely recognized, postpartum anxiety isn’t talked about nearly as much as it should be. Yet, studies suggest that anxiety symptoms are just as common—and in some cases even more frequent than depression. Naming and normalizing these experiences matters, because silence can make parents feel isolated when in reality, they are far from alone.
Noticing these symptoms isn’t a sign of weakness—it’s a sign that you may need and deserve extra support. Both PPD and PPA are treatable.
The Adjustment Into Motherhood
Motherhood changes everything—your time, your relationships, and even your sense of who you are. Many new parents describe the early days as both magical and disorienting.
And let’s be real: in those first few months, routines don’t really exist. Life revolves around unpredictable feeding times, short naps, and middle-of-the-night wake-ups. Days can blur together. The lack of structure can feel unsettling, especially if you’re someone who thrives on plans and predictability. Luckily, our babies are so cute—they keep us coming back for more, even when we haven’t slept in days.
Other common challenges include:
Loss of control: You can’t plan your day the way you used to.
Relationship shifts: Your partnership, friendships, and family dynamics may change in unexpected ways.
Overwhelm: The constant demands of caring for a baby can feel exhausting, even when done with love.
Experiencing any of these feelings or symptoms does not mean you are a bad mother. I know negative mom self-talk can be really loud, convincing you that you’re not doing enough—so feel free to reread these sentences as many times as you need: Recognizing your own needs and noticing when something feels off is a sign of strength—and it shows you are deeply attuned to both yourself and your baby. You are an amazing mother!
Your Body and Healing
Alongside all the emotional adjustments of postpartum life, your body is undergoing its own transformation and healing. Whether you had a vaginal birth, a C-section, or a combination of medical interventions, recovery takes time—sometimes much longer than anyone warned you about.
You might notice changes in strength, stamina, sleep patterns, and physical comfort. Everyday tasks may feel heavier or more exhausting than they used to. Even something as simple as standing up can be challenging when your abdominal muscles feel nonexistent. And seeing your body look or feel different can be emotionally challenging, especially when combined with the constant demands of caring for a newborn.
It’s important to remember: your body just accomplished something incredible. Healing doesn’t mean rushing back to your pre-pregnancy routine or appearance—it means honoring your body’s needs while gradually regaining strength and confidence.
This period can also impact your sense of identity. Feeling “off” in your own body may ripple into how you experience motherhood or even how you view yourself outside the role of parent. Being patient with yourself physically and emotionally is part of integrating your new life as a parent while nurturing yourself.
Practical ways to support your healing include:
Gentle movement (walking, stretching, or postpartum-approved exercises)
Adequate rest and sleep whenever possible
Nutrition that nourishes your body and supports recovery
Asking for help with lifting, carrying, or household tasks
Mindful moments to check in with how your body feels and what it needs
Recognizing that your body’s recovery is part of your broader adjustment to motherhood reinforces that both your physical and emotional well-being matter—and both deserve attention and compassion.
Shifting Self-Identity
Along with daily life changes comes a deeper shift in identity. You might ask yourself: Who am I now, beyond being a mom?
It’s normal to grieve the “old you” while also embracing your new role. You may feel a pull between wanting to hold onto your independence and pouring yourself into motherhood. This process, sometimes called matrescence (the transition into motherhood), can be as transformative and as complicated as adolescence.
In therapy, especially Dialectical Behavior Therapy (DBT), we often talk about dialectics: the idea that two opposing truths can exist at the same time. You can miss your old life and love your new one. You can feel exhausted and deeply connected to your baby. You can struggle and be doing an incredible job as a mother.
Your body may feel unfamiliar.
Career goals, hobbies, or social life may feel distant.
Your role within your family and community may evolve.
Holding space for these “both/and” truths can reduce shame and help you honor the complexity of your journey.
Moving Forward With Support
If you’re finding this season heavier than expected, reaching out for help is a sign of strength. Therapy, support groups, and leaning on loved ones can provide comfort and perspective.
And while self-care looks different now, it still matters. Sometimes it’s not bubble baths or long walks—it’s a 10-minute nap, a hot shower, or eating a real meal. Those small steps add up.
Motherhood was never meant to be done in isolation. With support, compassion, and time, you can find a rhythm that works for you and begin to feel like yourself again—just in a new, evolving way.
Gentle Reminders for New Moms
You can love your baby deeply and find this stage incredibly hard.
Rest is productive—your healing matters too.
Having needs doesn’t make you less of a mother; it makes you human.
Your baby doesn’t need a perfect mom—they need you.
Noticing when you’re struggling is a sign of strength, not weakness.
The days may feel long, but you are growing right alongside your baby.
It’s okay to miss your old self while also embracing your new identity.
You don’t have to do this alone—support is part of thriving.
Resources
If you or someone you love is struggling, here are places to turn for support:
Postpartum Support International (PSI): Call or text the HelpLine at 1-800-944-4773 (4PPD) or text “Help” to 800-944-4773.
988 Suicide & Crisis Lifeline: Dial 988 in the U.S. for immediate support if you are in crisis.
National Maternal Mental Health Hotline: 1-833-943-5746, available 24/7.
Talk with your OB-GYN, midwife, or primary care provider—they can connect you with local resources.
You are not alone. Help is out there, and healing is possible.
The Permission to Recharge: Why Slowing Down Feels So Hard
In a culture that glorifies hustle and productivity, slowing down often feels like failure. This blog explores why rest feels so hard, from scarcity culture and guilt to our addiction to busyness. Using the metaphor of a phone that can’t recharge while still in use, it illustrates the difference between “fake rest” that distracts us and “real rest” that restores us. Drawing on research and practical examples, the post highlights the seven types of rest—physical, mental, sensory, emotional, social, creative, and spiritual—and explains how each plays a vital role in well-being. Readers are encouraged to reflect on their own barriers to rest and given actionable ways to recharge, reminding them that rest isn’t something to be earned but a human necessity.
Why Rest Feels So Hard in a Hustle Culture
We live in a world that glorifies hustle. Phrases like “rise and grind” or “I’ll sleep when I’m dead” are worn like badges of honor. Rest, meanwhile, is often dismissed as laziness. This mindset is so normalized that slowing down can actually feel uncomfortable, even dangerous, as though we’re falling behind.
But the cost of constant motion is high. When we don’t allow ourselves to rest, we burn out—and burnout doesn’t just mean being tired. It can look like irritability, brain fog, difficulty focusing, lack of creativity, and even physical symptoms like headaches or digestive issues. Everything suffers: our work, our relationships, our health, and our sense of self.
One reason it’s so hard to embrace rest is that we’ve been taught to value productivity above all else. We often measure our worth by how much we’ve accomplished in a day, not by how we’ve cared for ourselves. If the to-do list isn’t finished, or the inbox isn’t cleared, we label the day a failure. Productivity becomes the standard of worthiness, and when we’re not producing, we feel guilty.
Why Is It So Hard to Slow Down?
Several forces make slowing down more difficult than it should be:
Scarcity culture whispers “never enough.” Brené Brown describes scarcity culture as the constant hum of inadequacy: not thin enough, not smart enough, not productive enough. When rest is filtered through this lens, it feels like proof we’re not doing enough.
We’re addicted to busy. Staying busy gives us a sense of control. It also distracts us from uncomfortable emotions—like loneliness, grief, or uncertainty—that might surface in the quiet moments.
We equate value with output. Many of us were taught that achievement equals worth. If we slow down, we fear it means we’re less valuable. This is especially true in environments (workplaces, schools, families) where constant achievement is praised, and rest is seen as weakness.
Understanding why rest feels difficult can help us begin to unlearn the naratives that keep us from it.
The Phone Metaphor: Recharge Effectively
Imagine your phone on 1% battery. You plug it in, but you also keep scrolling, streaming, texting, and opening apps. The battery climbs only a little, or sometimes not at all.
That’s exactly what many of us do with rest. We say we’re “recharging,” however we keep our brains busy—answering emails during a break, scrolling on social media in bed, or planning tomorrow’s to-do list while trying to “relax.” Just like the phone, we can’t actually refill our energy if we don’t power down.
True rest is like letting the phone sit quietly in the charger and letting our phone just be. It might feel uncomfortable at first, however that’s the only way to truly be able to fully recharge.
A Real-Life Example: “Fake Rest” vs. Real Rest
Think about this: Alex finishes a long workday and collapses onto the couch. They tell themselves they’re “resting,” but then they grab their phone, scroll through Instagram, answer a couple of Slack messages, and half-watch a show while making a mental list of tomorrow’s tasks. Two hours later, Alex is drained, overstimulated, and frustrated because they’re still tired.
That’s fake rest. It distracts, but it doesn’t restore.
Now imagine if Alex instead put their phone on “do not disturb,” dimmed the lights, and went for a slow walk outside. Afterward, they made tea, stretched for ten minutes, and let themselves journal about the day. That kind of rest might only take an hour, but it feels like a true reset.
The difference isn’t time—it’s intention. Fake rest numbs us; real rest restores us.
The Science of Rest
Rest isn’t indulgent—it’s biological.
Brain health: During downtime and sleep, the brain consolidates memories, processes emotions, and clears out waste. Without this, we struggle with concentration and emotional regulation.
Nervous system reset: Rest allows us to move from “fight or flight” mode into “rest and digest,” giving our bodies space to repair, regulate hormones, and strengthen the immune system.
Creativity and problem-solving: Ever notice how your best ideas come in the shower or on a walk? That’s because rest activates parts of the brain responsible for insight and creativity.
When we deny ourselves rest, we’re not only exhausted—we’re less effective at the very productivity we’re chasing.
The Seven Types of Rest
Real rest isn’t one-size-fits-all. Saundra Dalton-Smith identifies seven types of rest, and understanding them can help us pinpoint what we actually need:
Physical Rest – Includes sleep, naps, stretching, yoga, or simply lying down. For those with physically demanding jobs, this is essential.
Mental Rest – Stepping away from constant decision-making and problem-solving. This might look like journaling thoughts out of your head or giving yourself permission to not think about work after hours.
Sensory Rest – Our senses are bombarded all day with noise, screens, and notifications. Sensory rest means silence, dim lights, unplugging, or stepping outside.
Emotional Rest – Space to be authentic without needing to perform or please others. This might be talking honestly with a friend, seeing a therapist, or letting yourself cry.
Social Rest – Not all social time is restful. Social rest is choosing time with people who recharge you—or choosing solitude if that’s what you need.
Creative Rest – Feeding your soul with beauty and inspiration: walking in nature, looking at art, listening to music, or daydreaming.
Spiritual Rest – Connecting with meaning and purpose beyond yourself—through prayer, meditation, reflection, or simply aligning with your values.
Sometimes exhaustion isn’t about needing more sleep—it’s about needing the right kind of rest.
Barriers to Real Rest
Even when we know the importance of recharging, rest can still feel out of reach. Common barriers include:
Guilt: Many of us carry an internalized belief that rest has to be earned, so downtime feels selfish.
Perfectionism: We tell ourselves we can rest after everything is done—but in reality, the list never ends.
Numbing instead of resting: Scrolling, binge-watching, or online shopping give temporary relief but don’t restore us. They’re distractions, not true rest.
Fear of falling behind: Resting can spark anxiety that someone else is working harder, getting further, or achieving more while we pause.
By noticing these barriers, we can gently challenge them instead of automatically believing them.
Practical Ways to Recharge
Allowing yourself to recharge doesn’t always mean booking a spa day or a vacation (though those are wonderful). Small daily practices can create the space you need to restore:
Take a walk outside without headphones, letting your mind wander.
Sit down for a meal without your phone, focusing only on eating.
Create “do not disturb” hours for your phone and email—especially before bed.
Schedule rest into your calendar as a non-negotiable appointment.
Use micro-breaks: just two to five minutes of breathing, stretching, or looking out a window.
Practice a hobby purely for enjoyment, not to achieve or improve.
Try a bedtime ritual that signals your body it’s time to wind down (reading, gentle stretching, journaling).
Think of these not as luxuries, but as maintenance, the same way charging your phone is. We need to be able to give ourselves the space to recharge in order to more effectively function in our day to day life.
A Gentle Reminder
When we truly allow ourselves to pause, not just plug in while still running, we give our minds and bodies the space they need to repair, reset, and come back stronger.
Rest is not something that you need to earn. You’re allowed to recharge simply because you’re human.
Slips, Lapses, and Relapses: Why ED Recovery Isn’t a Straight Line
Recovery isn’t a straight line—and that’s okay. Along the way, slips, lapses, and relapses may happen, but they don’t erase your progress. Every bump in the road is an opportunity to learn, reroute, and keep moving forward. No matter how messy recovery feels, healing is still happening.
Recovery isn’t a straight line, as much as we may like it to be.
Detours happen. Emotions come up. Old patterns can resurface. And when they do, it can feel discouraging, even scary, like you’ve “messed up” or “gone backwards.” It’s important to not give into these thoughts and remember that healing is still happening, even when it feels messy.
In eating disorder recovery, it’s important to understand the difference between slips, lapses, and relapses—because not every setback means you’re back at square one.
What does it mean to be “in recovery”?
Being “in recovery” from an eating disorder can mean different things to different people. For some, recovery is about no longer engaging in disordered behaviors—a focus on food freedom and body trust. For others, recovery is about working toward peace with food and body, even if thoughts still pop up from time to time.
Recovery might mean:
Learning how to eat regularly and consistently
Challenging food rules and fears
Reconnecting with your body’s cues for hunger and fullness
Replacing shame with compassion
Building a life that feels bigger than the eating disorder
It’s not a single finish line—it’s a process. And just because your version of recovery doesn’t look like someone else’s doesn’t mean it’s “less valid.”
Recovery isn’t all-or-nothing
This is where many people get stuck: they assume recovery means never struggling again. But the reality is, recovery often includes slips, lapses, and sometimes even relapses. These moments don’t cancel out your progress—they’re simply part of the journey.
In fact, setbacks can become some of the most valuable parts of recovery. Each time you slip or lapse, you’re given the chance to practice responding differently than you would have in the past. Struggle isn’t proof of failure—it’s an opportunity to strengthen your ability to navigate life in recovery and build resiliency.
Slips, Lapses, and Relapses
Slip – A slip is a small, brief return to an old behavior. Maybe you skip a snack, overexercise one day, or find yourself using a disordered thought pattern in a stressful moment. Slips happen. They don’t erase your progress.
Lapse – A lapse is a little bigger than a slip. It might last longer, or involve more than one behavior. Think of it as a bump in the road rather than a full detour. You may feel shaken, but you can still course-correct quickly with support and compassion.
Relapse – A relapse means returning more consistently to disordered patterns and stepping away from your recovery tools. It doesn’t mean you’ve failed—it just means extra support is needed to get back on track.
Why naming this matters
When you can identify what’s happening, you take back power from shame. A slip doesn’t have to spiral into a relapse. A lapse doesn’t undo months of progress. Recovery is about learning to notice, name, and respond differently each time.
Recovery Has No Timeline
It’s so easy to fall into the trap of comparing your recovery to someone else’s. Maybe you’ve heard stories of people who “just stopped” their eating disorder behaviors and never looked back, or you’ve seen others who seem to move forward without stumbling. That can make your own ups and downs feel discouraging.
It’s important to remember that everyone’s recovery timeline is unique. For some, progress feels steady. For others, it feels like two steps forward, one step back. Neither is wrong. Healing isn’t about speed or how “linear” it looks—it’s about continuing to return to your values and your recovery goals, no matter how many times you need to reroute.
Recovery isn’t a race. There’s no finish line you have to cross in a certain amount of time. What matters most is that you keep showing up for yourself, again and again.
Recovery as a road trip
Think of recovery like going on a cross-country road trip. You’ve left your starting point behind (living fully in the eating disorder) and you’re on your way to a new destination (freedom, peace, and trust with yourself).
Along the way, things might not always go as planned—you could hit construction, run into bad weather, or take a wrong exit. These detours might slow you down, however they don’t teleport you back to where you started. You’re still on the road, still moving forward, still closer to your destination than when you began.
What to do when a setback happens
Pause and check in with yourself—what triggered the slip or lapse?
Practice self-compassion instead of shame.
Look for the lesson: what can this experience teach you about navigating challenges in the future?
Reach out to your support system or treatment team.
Remind yourself: This is part of the process. I am still moving forward.
Planning Ahead in Recovery
While slips, lapses, and relapses can happen, it doesn’t mean we’re powerless. One of the most empowering parts of recovery is learning how to plan for challenges before they come up.
When we think about recovery as a journey, part of the road trip is packing wisely—knowing what you might need if detours show up. This doesn’t mean you’re expecting yourself to “fail,” rather setting yourself up with tools and supports to lean on if obstacles do show up. Think of it like packing an extra change of clothes that you might not need; however you want to have just in case.
Some things you might include in your ED recovery plan:
Recognizing triggers – Certain environments, stressors, or emotions may make urges stronger. Naming these ahead of time takes away their power to surprise you.
Identifying early warning signs – Maybe you notice more food/body thoughts, increased anxiety, or urges to isolate. Catching these early gives you the chance to respond before behaviors take hold.
Choosing how to respond – Planning grounding tools, coping strategies, or who you’ll reach out to if you notice a slip can help you shift back into a recovery mindset more quickly.
Naming ways to not respond - Identifying unhelpful and maladaptive coping skills and behaviors that lead you further away from the recovery path
Using your support system – Sharing your plan with a therapist, dietitian, or trusted friend helps you feel less alone and makes it easier to ask for support when you need it.
Recovery planning is about building resilience, not perfection. Every time you practice noticing triggers and responding differently, you strengthen your recovery muscles. Just like a road trip, the more maps and tools you bring along, the more confident you feel navigating whatever comes your way.
Common Myths About ED Recovery
Myth 1: Recovery means I’ll never have food or body image struggles again.
Recovery doesn’t erase every hard thought—it changes your relationship to them. You can have a thought without acting on it.Myth 2: If I slip, I’ve ruined my recovery.
Not true. Slips are normal and expected. They’re information, not proof of failure.Myth 3: Everyone’s recovery should look the same.
Your recovery is unique. Comparing your timeline to someone else’s only fuels shame—it doesn’t speed up healing.Myth 4: Recovery should feel linear and steady.
In reality, recovery often feels like two steps forward, one step back. Progress is measured over time, not in a single moment.
The bigger picture
Being in eating disorder recovery doesn’t mean you never struggle. It means you are committed to showing up, trying again, and building a healthier relationship with yourself.
Healing isn’t about perfection. It’s about persistence. Each struggle is not a reset, but a chance to grow stronger and prepare for the road ahead.
So when slips, lapses, or even relapses happen, remember: you are still doing the work. You are still moving forward. Be gentle with yourself. Keep going.
Recovery is not about never falling, but about learning how to stand up again and again. Every step forward counts, even if it feels small.
ADHD & Perfectionism: A Hidden Struggle
ADHD and perfectionism may seem like unlikely companions- after all, ADHD is often associated with disorganization, impulsivity, and inattention, while perfectionism is about control, precision and high standards. Yet, many people with ADHD struggle with a form of perfectionism that can be both paralyzing and self-sabotaging.
You go to put a stack of clean clothes away in your closet. Simple enough, right? But as soon as you open the door, you notice the hangers are mismatched, the shoes are a mess on the floor, and suddenly it feels like you can’t just put the clothes away—you need to reorganize the entire closet.
And then? You shut the door and walk away. The clothes sit in a pile, and the shame starts creeping in.
That’s ADHD perfectionism in action. On the surface, ADHD and perfectionism don’t sound like they’d go together. ADHD is often described as impulsive, scattered, forgetful. Perfectionism sounds like the opposite: precise, controlled, flawless. But for many people with ADHD, the two are deeply connected—and perfectionism often serves a function.
What Is Perfectionism?
Perfectionism is more than just “wanting to do well.” At its core, it’s the belief that anything less than flawless is unacceptable. It often shows up as:
Unrealistic expectations: Expecting yourself to achieve more than what’s humanly possible.
Fear of mistakes: Viewing errors as failures instead of learning opportunities.
Tying worth to performance: Believing your value comes only from what you accomplish.
All-or-nothing thinking: If something isn’t perfect, it feels like it doesn’t count at all.
Perfectionism is the voice that says:
“If it’s not flawless, it doesn’t count.”
“If I make a mistake, I’ve failed.”
“I’ll only be worthy if I do this perfectly.”
It ties your self-worth to performance and sets the bar impossibly high. And while it can sometimes push you to do great work, most of the time it leaves you anxious, procrastinating, self-doubt, intense pressure and falling into cycles of avoidance.
How Perfectionism Functions in ADHD
For someone with ADHD, perfectionism can act as both a shield and a coping strategy. Many people with ADHD grow up hearing they are “careless,” “lazy,” or “not living up to potential.” Striving for perfection becomes a way to prove those labels wrong.
A shield against criticism: If something is perfect, no one can call it sloppy or incomplete.
A way to find structure: ADHD brains crave clarity. Believing there’s a “perfect” way to do something can simplify choices and reduce overwhelm.
An energy driver: Sometimes the only way to spark motivation is by holding yourself to the highest possible standard, even if it’s unsustainable.
But perfectionism comes with a hidden cost. The pressure to do something perfectly often leads to procrastination—if it can’t be done flawlessly, it feels safer not to start at all. That creates a frustrating cycle of avoidance, missed deadlines, and guilt, feeding right back into the ADHD shame spiral.
Perfectionism and Rejection Sensitivity
One of the lesser-talked-about ADHD traits is rejection sensitivity—a heightened emotional response to real or perceived criticism, rejection, or disapproval. For many with ADHD, rejection doesn’t just sting; it feels crushing.
Perfectionism becomes a defense mechanism against that pain. If the work, the project, or even the way you show up in relationships is “perfect,” then maybe there won’t be room for rejection. It’s an attempt to shield yourself from the heartbreak of being told you’re not enough.
Of course, this isn’t foolproof. Perfection doesn’t guarantee acceptance, and the pressure of maintaining it can be exhausting. Still, the drive for flawlessness often makes sense in the context of protecting against rejection sensitivity.
The Brain-Based Side of Perfectionism in ADHD
ADHD isn’t just about willpower—it’s about brain wiring. Perfectionism often develops as a way to navigate some of these neurobiological realities:
Executive function challenges: ADHD impacts planning, organization, and task initiation. If these skills feel shaky, the brain compensates by clinging to rigid standards—“If I can just do it perfectly, maybe I can keep things under control.”
All-or-nothing thinking: ADHD brains often swing between extremes. Either you’re hyper focused and producing amazing work, or you’re stuck in paralysis. Perfectionism feeds this cycle—if it can’t be all the way “on,” it feels impossible to even start.
The dopamine connection: ADHD brains struggle with motivation when tasks don’t feel immediately rewarding. Perfectionism creates a high-stakes environment that can trigger dopamine—waiting until the last minute, pushing for flawless results, or chasing the “perfect” idea can all give a rush of urgency and focus.
Heightened emotional regulation difficulties: Criticism feels more intense for ADHD brains, so perfectionism is used as a buffer to avoid the flood of emotions that comes with rejection or disappointment.
In other words: perfectionism in ADHD isn’t just a personality quirk—it’s a brain-based survival strategy.
The ADHD + Perfectionism Cycle
Here’s how the cycle often plays out:
Imagine starting a task with good intentions, but then noticing it’s not “perfect.” That perfectionistic voice spikes anxiety and self-criticism, making you feel like you’re failing. For someone with ADHD, this can trigger procrastination, distractibility, or hyper-focus on tiny details instead of finishing the task. Avoidance or overcompensation follows—maybe you reorganize your desk, rewrite a draft, or endlessly tweak a project—temporarily relieving stress but not completing the work. The more the task feels “impossible,” the more ADHD-related challenges surface, feeding the perfectionism even further. This creates a repeating loop: ADHD makes perfection hard to achieve, and perfectionism amplifies ADHD struggles, leaving motivation and confidence drained.
Start task with good intentions→ often with unrealistic expectations
Perfectionism kicks in → task feels “wrong” or “not good enough”
Anxiety & self-criticism rise → ADHD symptoms increase (distraction, procrastination, hyper-focus)
Avoidance or overcompensation → reorganizing, tweaking, delaying
Temporary relief but no progress → feeds back into perfectionism
This loop is exhausting—but also very common for ADHD brains. Naming it is the first step to breaking it.
Common myths about ADHD and perfectionism
Myth: “People with ADHD don’t care about details.”
Reality: Many care deeply—but fear of not getting it right often keeps them from even starting.
Myth: “ADHD is all chaos, perfectionism is all control—they can’t coexist.”
Reality: They coexist often. Perfectionism is a coping mechanism to create order in the chaos.
Myth: “Perfectionism means you’re just being too picky.”
Reality: For ADHD, perfectionism usually comes from fear—of mistakes, of criticism, of rejection—not from fussiness.
Everyday ways this shows up
Perfectionism in ADHD often shows up in everyday life in ways people might not expect:
Cleaning the house: You avoid starting because you believe you need hours to do it “the right way”—every corner spotless, every drawer organized. So the dishes pile up, and the task feels heavier each day.
School or work projects: You spend hours tweaking fonts, formatting, or re-writing one sentence instead of finishing the assignment, because it has to be “just so.”
Emails or texts: You rewrite a simple message five times before sending, worrying it might be misunderstood or sound “wrong.”
Creative projects: You never share your art, writing, or music because it doesn’t feel “ready” yet—and sometimes it never gets shared at all.
Practical Strategies for Loosening Perfectionism’s Grip
Letting go of perfectionism doesn’t mean giving up on quality. It means creating space for flexibility, self-compassion, and realistic expectations. Here are a few ways to start:
Redefine “done.” Instead of asking, “Is this perfect?” ask, “Is this complete and good enough to serve its purpose?”
Use time limits. Give yourself a set amount of time to work on something, and when the timer goes off, move on—even if it feels unfinished.
Shrink the task. Instead of cleaning the whole house, commit to doing the dishes for five minutes. Often, starting small breaks the avoidance cycle.
Challenge the “what ifs.” Ask yourself, “What would actually happen if this isn’t perfect?” Most of the time, the consequences are far less severe than the perfectionist brain imagines.
Practice self-compassion. Remind yourself that mistakes are part of learning—and that imperfection doesn’t erase your worth.
Celebrate progress, not perfection. ADHD brains thrive on reward—acknowledge small wins so the brain starts associating progress with positive reinforcement.
Final Thoughts
ADHD and perfectionism may seem like opposites, but they are often deeply intertwined. Perfectionism can serve as a way to manage overwhelm, shield against criticism, and protect from rejection sensitivity. On a brain-based level, it also provides dopamine boosts, compensates for executive function struggles, and offers a sense of control in an unpredictable world.
The trick is learning when it’s helping you—and when it’s keeping you stuck. Because at the end of the day, “good enough” really is enough. And often, it’s the thing that finally gets you moving forward.
Setting Boundaries — Why Pushback is Normal
Setting boundaries is an act of self-respect—but it often comes with resistance. When you begin saying “no” or protecting your time, others may push back, not because you’re wrong, but because they’re adjusting to a new pattern. Just like giving a child a new bedtime, change can feel uncomfortable at first. With consistency and compassion, boundaries create healthier relationships and more space for your own well-being.
When you first start setting boundaries, you may notice resistance. Friends, family, or coworkers may react with frustration, confusion, or even anger. This often leaves people wondering: Am I doing something wrong?
The truth is, pushback is normal — and often a sign that you’re creating healthy change. Boundaries aren’t about being harsh; they’re about honoring your own needs, time, and energy. At their core, they are an act of self-respect.
Why Boundaries Are Important — and How They Strengthen Relationships
At first, boundaries can feel like walls. You may worry that saying no or protecting your time will push people away. But the truth is the opposite: healthy boundaries create stronger, more respectful, and more authentic connections.
Here’s why:
They Build Trust.
When you’re clear about your limits, others know where they stand with you. They don’t have to guess what’s “too much” or worry they’re crossing invisible lines. That clarity fosters safety and mutual respect.They Reduce Resentment.
Without boundaries, it’s easy to overextend yourself — and then feel drained, taken advantage of, or resentful. Boundaries prevent burnout, which allows you to show up for others with more genuine care.They Encourage Mutual Respect.
When you honor your own needs, you model self-respect. Over time, others learn to respect your limits — and it gives them permission to honor their own as well.They Create Space for Authenticity.
Relationships thrive when people can show up as their true selves. Boundaries protect that authenticity by ensuring you’re not just going along to keep the peace. They let you say, “This is who I am, and this is what I need.”They Deepen Connection.
Far from pushing people away, boundaries allow for more meaningful closeness. Instead of being built on obligation or guilt, the relationship is grounded in honesty, consent, and mutual care.
The Bottom Line: Boundaries aren’t about shutting people out. They’re about creating relationships where both people feel respected, valued, and safe. Healthy boundaries free you from resentment and invite others into more authentic, balanced connection.
Why Pushback Happens
People become accustomed to the roles we play and the access they’ve had to our time, energy, and emotional labor. When you shift those patterns, it can feel disruptive to them, even if the new boundary is healthier for you both.
Think of it like this: Setting a boundary is like giving a child a bedtime when they’ve never had one before. At first, there may be protests. They might argue, cry, or test limits — not because the bedtime is bad, but because it’s new. Over time, structure creates safety and well-being.
The same thing happens with adults. When you begin setting boundaries, people who are used to unlimited access to you may resist. They might push back, guilt-trip, or try to test the limits — not necessarily because your boundary is unfair, but because it’s unfamiliar. Just like children eventually adjust and even thrive within structure, adults in your life can also learn to adapt to your boundaries over time.
When you establish a limit, you’re not only protecting yourself — you’re also teaching others how to treat you. This is self-respect in action: showing that your needs and well-being are just as important as anyone else’s.
What Pushback Really Means
It’s not a sign that your boundary is wrong.
It’s a sign you’re disrupting an old pattern.
It’s a chance to practice self-respect and remind yourself that your worth isn’t defined by pleasing others.
It’s an opportunity for growth — for you and your relationships.
Facing pushback can be tough. However, it’s essential to hold steady with the boundary you’ve set. If we back down each time resistance shows up, we may unintentionally be communicating that our boundaries aren’t actually serious, and that future ones can also be tested or ignored. When pushback happens, it’s helpful to come back to your why: the reason you set the boundary in the first place. Boundaries aren’t about punishment; they’re about protecting your well-being and creating the foundation for healthier, more fulfilling relationships.
How to Set Boundaries When There’s Pushback
Stay calm and consistent. Don’t match the intensity of the pushback. Hold your boundary with steady confidence.
Example: “I understand this is frustrating, but I won’t be available to talk after 9 p.m.”
Use clear, simple language. Avoid over-explaining or apologizing excessively. Boundaries don’t require justification to be valid.
Example: “I can’t lend money right now.” (You don’t need to give 10 reasons why.)
Acknowledge their feelings, but don’t bend. Empathy can soften resistance, but it doesn’t mean giving in.
Example: “I hear that this is hard for you, and I still need to stick with what I said.”
Remind yourself why you set the boundary. Boundaries are about your well-being, not controlling others’ comfort.
Practice self-respect. Each time you enforce a boundary, you reinforce the truth: My needs are important, and I deserve to honor them.
The Takeaway
Boundaries are not about building walls — they’re about choosing self-respect, clarity, and healthier connections. If you experience pushback, remember: the discomfort is temporary, but the benefits — stronger relationships, more peace, and greater authenticity — are lasting.
Every time you set a boundary, you reinforce the message: My needs matter. I respect myself enough to protect them.
Living With Intention — Steering Your Own Ship
Living with intention is about choosing your own course, even when life’s currents feel out of your control. Instead of drifting aimlessly, intentional living helps you align your actions with your values, creating a sense of purpose and direction. Like steering a ship, you may not control the waves, but you can chart a path that feels steady, meaningful, and truly your own.
Many of us go through life on autopilot: answering emails the moment they arrive, saying yes before we pause to think, or scrolling endlessly without noticing time pass. Autopilot can feel efficient, but often, it pulls us away from what truly matters. We may end the day feeling busy but empty, reacting to life rather than shaping it.
Have you ever driven somewhere and suddenly realized you arrived without remembering the drive itself? That’s a perfect example of autopilot: moving forward, but not fully aware or present. The same can happen in life—days, weeks, or even months can slip by without us noticing if our actions align with our values.
What It Means to Live Intentionally
Living with intention doesn’t mean controlling every detail of life. It’s not about perfection, over-planning, or rigid routines. Instead, it’s about pausing long enough to notice your options and make conscious choices instead of letting life make them for you.
Intentional living is:
Saying yes to what aligns with your values. This could be dedicating time to a creative hobby, nurturing meaningful relationships, or taking on work that feels purposeful.
Saying no to what drains you. Protect your energy by turning down obligations, social invitations, or habits that don’t serve your goals.
Creating space for people, practices, and goals that matter most. Whether it’s scheduling weekly time for self-reflection, exercise, or connecting with loved ones, intentional living requires deliberate space-making.
A Helpful Metaphor
Imagine you’re in a boat without a paddle. You may drift quickly, but the current decides where you go. That’s life on autopilot: fast, reactive, and often misaligned with your deeper goals.
Now imagine picking up the paddle. You can’t control the waves or the current, but you can steer toward what matters. Some days, the paddle will feel heavy, and progress may be slow—but even a small adjustment in direction keeps you moving toward your values.
Small Actions, Big Impact
Intentionality doesn’t require giant life changes. It can start with a single daily choice:
Taking a five-minute pause before replying to a stressful email.
Choosing to walk outside instead of scrolling on your phone.
Reflecting on your day before bed: “Did my actions today reflect my values?”
Each small choice strengthens your ability to navigate life with awareness and purpose.
7-Day Intentional Living Challenge
Start steering your life toward what truly matters with this simple, week-long challenge. Each day focuses on a small, intentional action to build awareness and momentum.
Day 1: Pause Before You Respond
Before answering any email, text, or request today, take a deep breath and ask: “Does this align with my priorities or values?” Respond consciously rather than automatically.
Day 2: Identify One Energy Drainer
Notice one activity, obligation, or habit that consistently drains you. Today, say “no,” delegate it, or limit it. Track how it feels to reclaim this energy.
Day 3: Schedule Something Meaningful
Block out at least 30 minutes for something that nurtures your values—reading, a walk, creative time, connecting with a loved one. Treat it as non-negotiable.
Day 4: Reflect and Journal
Spend 10 minutes journaling about your choices today. Did they reflect your values? What felt aligned, and what felt automatic or reactive?
Day 5: Mindful Movement
Incorporate intentional movement today—yoga, stretching, or a walk—while fully noticing your body and surroundings. Focus on being present rather than rushing through.
Day 6: Declutter One Space
Pick one area—your desk, email inbox, or a drawer—and intentionally clear it. Physical decluttering reinforces mental clarity and the habit of conscious choice.
Day 7: Celebrate Small Wins
Reflect on the week. Identify 2–3 intentional choices you made that felt meaningful. Celebrate them—this reinforces your capacity for deliberate action and builds momentum.
Tip: After the week, repeat the challenge, gradually adding more intentional choices. Over time, these small actions become habits, helping you live with direction rather than drift.
Reflection Questions: Finding Your Autopilot Moments
Take a few minutes to answer these questions to identify where you’ve been drifting and where to start paddling:
When today or this week, did you act automatically rather than intentionally?
What activities or obligations consistently leave you feeling drained or misaligned?
Which moments brought you energy, joy, or a sense of purpose?
If you could steer your life in one direction this week, what small action would you take today to begin that course?
The Takeaway
You don’t need to control everything. You just need to steer. Living with intention means noticing the currents of your life and making conscious choices, even when the waves feel strong. Every choice — no matter how small — is a step toward a values-driven, fulfilling life.
Start today: pick one area where you’ve been drifting—maybe it’s your mornings, your work, or your social time. Pause, reflect, and choose one intentional action that aligns with your values. Steering your course doesn’t require perfection, only awareness.
ADHD, Goal Setting & the Fear of Losing Momentum
Living with ADHD often means riding waves of motivation that can feel unpredictable. Many people fear that if they pause while working toward a goal, they’ll lose momentum and never start again. This blog explores why that fear exists, how “all-or-nothing” thinking shows up, and practical strategies to build restart points, trust natural rhythms, and make progress without burning out.
Living with ADHD often means living with big dreams and just as big frustrations. You might have heard—and even tried—the classic advice: “Break big goals into small steps.”
And yet… even when you know that strategy works, you might avoid it. Why?
For many people with ADHD, there’s a hidden fear at play:
“If I stop, I might never start again.”
That worry can shape the way you approach motivation, productivity, and even your sense of self-trust. Let’s break down why this happens—and what can help.
The “All-or-Nothing” ADHD Mindset
When you finally catch a wave of focus, it feels precious. You ride the momentum hard, because deep down you worry: “If I pause, I’ll lose it.”
This can lead to pushing yourself until exhaustion, skipping breaks, or resisting small steps in favor of “one big push.”
The reality is:
Momentum does sometimes fade.
That doesn’t mean you’ve failed.
It means your brain works in rhythms, not in straight lines.
The Avoidance Cycle
Another layer of this struggle is the avoidance cycle. When a task feels overwhelming—or when the fear of losing momentum kicks in—it’s easy to avoid starting altogether. Avoidance is one of those coping strategies that feels good in the moment but costs us more over time. So while avoidance is often used as a coping strategy, it is important to remember that it is a maladaptive way to cope despite the instant gratification we might feel in the moment.
Here’s how the cycle plays out:
Event – Something comes up that feels overwhelming, stressful, or uncomfortable. (Example: a big work task, paying bills, or even putting clothes away.)
Discomfort – Anxiety, fear, self-doubt, or overwhelm sets in. The body and brain signal: “This feels bad. Let’s escape.”
Avoidance – We decide to delay or not do the task. Maybe we scroll, distract, or walk away.
Instant Relief – For a short while, it feels better. The stress quiets down and we feel like we’ve escaped the pressure.
Increased Stress & Shame (Long-Term) – The problem hasn’t gone away; it’s still waiting. Now, guilt, shame, and more pressure build on top of the original discomfort.
Then the cycle repeats. Each time we avoid, the momentary relief teaches our brain that avoidance works—even though the long-term cost is higher. Over time, the discomfort and shame multiply with each round. That makes the task feel bigger, scarier, and more loaded the next time we face it. It’s not just about the task anymore—it’s also about the shame of not doing it earlier.
Avoidance works in the short term because it relieves the pressure. Think about doing the dishes. At first, leaving them in the sink feels easier than tackling them right away. Avoiding them brings a quick wave of relief.
But the longer you wait, the more the pile grows—and the harder it feels to start. Suddenly, a simple 5-minute task looks like a mountain. We go from a couple dishes in the sink, to a sink filled with dishes overflowing on to the countertops.
ADHD often magnifies this pattern. Small steps get delayed until they feel impossible. Avoidance builds on itself. And shame starts to whisper: “Why can’t I just do this?”
Shame & ADHD
This is where the shame spiral kicks in. Many people with ADHD grow up hearing they’re “lazy,” “unmotivated,” or “inconsistent.” So, when momentum slips, shame rushes in to confirm those old stories. This ends up feeding into shame.
When we buy into shame’s narrative (“I’m lazy,” “I’ll never get it together,” “Something’s wrong with me”), it chips away at self-esteem in a few ways:
Identity fusion: Instead of seeing a behavior (“I avoided that task”), shame convinces us it’s an identity (“I am a failure”).
Erosion of self-trust: Each time shame takes over, it feels harder to believe we can follow through next time.
Internalized criticism: Over time, the voice of shame can sound like our default inner voice, making self-compassion feel unnatural or even undeserved.
The result? A fragile sense of self-worth that feels conditional on productivity or perfection.
When we replace shame with curiosity and compassion, the opposite happens:
Self-esteem strengthens (“I can struggle and still be worthy”).
Motivation shifts from fear-driven to values-driven (“I want to move toward what matters, not just away from failure”).
The avoidance cycle weakens, because mistakes become learning moments instead of proof of inadequacy.
Reframes can look like:
Avoidance is not laziness—it’s a coping strategy.
Shame is not proof of failure—it’s a signal you need more compassion, not criticism.
Progress isn’t erased because you paused—you can always re-enter.
Instead of helping us “try harder,” shame drains energy, focus, and hope. Feeding into shame erodes self-esteem and sabotages motivation by keeping you stuck in avoidance—whereas compassion restores trust in yourself and makes small, sustainable action possible.
Willingness vs. Waiting for Motivation
One powerful skill for breaking the cycle is willingness.
Instead of waiting for the perfect wave of motivation, willingness asks:
Am I willing to take one small step, even if I don’t feel like it right now?
This could look like:
Washing just one plate instead of the whole sink.
Opening your computer, even if you’re not ready to write.
Setting a timer for 5 minutes to “just start.”
Willingness lowers the stakes. It builds trust that you can move forward without waiting for the “perfect” mindset.
Practical Tools to Break the Cycle
1. Name the Fear
When you catch yourself hesitating, say it out loud:
“I’m afraid to stop because momentum matters to me.”
“This isn’t procrastination, it’s me protecting my focus.”
Naming it softens the shame.
2. Create Gentle Restart Points
Think of these as bookmarks for your brain.
“Next time, I’ll just open the file.”
“Tomorrow, I’ll reread the last sentence I wrote.”
Restart points reduce the pressure of “starting from scratch.”
3. Practice Willingness
Ask yourself: “What’s the smallest step I’m willing to take right now?” Then do only that.
4. Trust the Cycle
Focus will ebb and flow. That’s ADHD reality—not a personal flaw. Remind yourself:
Pausing is not quitting.
Breaks protect energy.
Momentum can be rebuilt again and again.
Final Takeaway
If you live with ADHD, you don’t have to finish everything in one sitting. You don’t have to fear pauses. You don’t have to drown in shame when motivation slips.
Your progress doesn’t have to look perfect to be meaningful. With willingness, gentle restart points, and a compassionate view of the cycle, you can move toward your goals—without burning yourself out in the process.
Let’s Talk About Body Image
In a world filled with edited images and unrealistic beauty standards, it’s no wonder so many of us struggle with body image. But your worth has never been tied to numbers on a scale or how you compare to what you see online. Healing begins when we shift the focus away from changing our bodies and toward changing the pressures around us—cultivating compassion, rejecting harmful media messages, and understanding where we fall on the body image spectrum.
Because how you see yourself matters, and you’re not alone in the struggle.
Every day, people of all shapes, sizes, and backgrounds silently wrestle with body image. In a culture filled with filtered photos, comparison traps, and unrealistic standards, it’s easy to feel like your body isn’t “enough.”
You might sometimes feel like your body isn’t enough, but your worth has never been about numbers, sizes, or chasing perfection.
What Body Image Really Means
Body image is more than just how you look. It’s how you see, feel, and think about your body.
It includes your self-talk when you look in the mirror.
It shows up in how comfortable you feel in clothes, social settings, or even in your own skin.
It can shape your confidence, relationships, and mental health.
When body image turns harsh or critical, it can chip away at self-worth and feed patterns of shame, dieting, or self-punishment.
The Real Problem: Pressure, Not Your Body
We live in a culture that often glorifies thinness, perfection, or “transformation” as the ultimate goal. Social media filters, curated images, and comparison culture reinforce the lie that there’s only one acceptable way to look.
But the truth is:
Your body doesn’t need to change. The pressure does.
It’s the unrealistic standards that are harmful, not your body.
Scarcity Culture and Body Image: Why “Never Enough” Keeps Us Stuck
Brené Brown describes scarcity culture as the constant hum of “never enough.” We wake up thinking we didn’t get enough sleep, spend the day worrying we’re not productive enough, and fall asleep convinced we didn’t accomplish enough. This mindset doesn’t just shape how we measure success—it seeps into how we see ourselves, especially our bodies.
When scarcity culture meets body image, it can sound like this:
I’ll never be thin enough.
I’ll never be toned enough.
I’ll never look young enough.
I’ll never be disciplined enough to “stick with it.”
The rules keep shifting, and the finish line keeps moving. No matter how hard we try, it feels like there’s always another flaw to fix, another standard to chase. Our bodies stop feeling like home and start feeling like projects under construction.
The cruel part? Shame and scarcity feed each other. The more inadequate we feel, the more we double down on diets, punishing workouts, or self-criticism—hoping that this time, if we just work harder, we’ll finally feel enough. But that sense of worthiness never arrives, because the culture we’re swimming in is designed to keep us striving and unsatisfied.
Eating Disorders, Media, and Body Image: The Messages We Absorb
We don’t develop eating disorders in a vacuum. While genetics, trauma, and environment all play a role, the culture we live in—especially the media we consume—shapes how we see our bodies and what we believe about our worth.
From magazine covers to TikTok trends, we’re flooded with narrow and unrealistic standards of beauty. Thinness is celebrated. “Clean eating” and hyper-fitness are praised. Filters and editing erase natural bodies and turn them into impossible ideals. The message we receive, over and over, is: your body is not enough as it is.
For someone vulnerable to disordered eating, these messages can act like fuel. A perfectly normal body suddenly feels unacceptable. Food becomes a battleground. Exercise becomes punishment instead of self-care. And the cycle of shame, restriction, and overcompensation deepens.
The impact doesn’t stop with individuals—it becomes cultural. Media creates a hierarchy of bodies: thin over fat, youthful over aging, “fitspo” over rest. This hierarchy reinforces Brené Brown’s idea of scarcity culture, the sense that no matter what we do, we’ll never measure up.
Unfortunatly we start to forget that bodies in the media are not reality. They’re curated, edited, and filtered to keep us striving (and buying). And striving for an impossible standard is exactly what keeps us stuck in the loop of body dissatisfaction and, for many, eating disorders.
Understanding the Body Image Spectrum
Body image isn’t just “good” or “bad.” It exists on a spectrum, and people may move between different points depending on the day, the season of life, or their healing journey.
Here’s a simplified way to think about it:
Negative Body Image
Feeling uncomfortable in your body
Harsh self-criticism and shame
Preoccupation with appearance or size
Body Neutrality
Shifting focus from looks to function
Recognizing, “My body lets me walk, breathe, hug, and live.”
Accepting that you don’t have to love every part of your body to treat it with care
Body Respect & Body Acceptance
Meeting your body with care, regardless of appearance
Nourishing and resting your body because it deserves it
Building sustainable self-compassion instead of conditional acceptance
Body Positivity
Actively celebrating body diversity
Challenging beauty standards and embracing differences
Reframing your body as worthy of joy, pleasure, and representation
Wherever you find yourself on this spectrum, it’s important to remember: none of these points are about perfection. They’re about relationship. And like any relationship, it can evolve over time.
Shifting Toward Healing
Healing body image isn’t about “learning to love every part of yourself overnight.” It’s about building a kinder, more compassionate relationship with yourself over time.
Here are a few gentle starting points:
Notice your self-talk. When you catch harsh inner criticism, pause and ask, “Would I speak this way to a friend?”
Appreciate function over form. Your body allows you to breathe, laugh, hug, and move through the world. Gratitude for what your body does can soften how you feel about how it looks.
Build media literacy. Notice when images are edited or filtered and remember, comparison is unfair when the standard isn’t real.
Diversify your feed. Follow accounts that celebrate body diversity, recovery, and authenticity.
Call out diet culture. When you see media praising restriction or shaming bodies, recognize it as harmful messaging not truth.
Practice self-compassion. Healing begins with kindness towards yourself. This means meeting yourself with patience on the tough days, and reminding ourselves that our worth is not up for debate, no matter what the media tells you.
You’re Not Alone
If you struggle with body image, know this: you are far from alone. Many people carry the same quiet battle — but silence makes it heavier.
The more we name these pressures, challenge them, and support each other, the more freedom we can create.
Your worth is not defined by a number, a size, or a reflection. You deserve to live in your body without shame — and to meet yourself with the same compassion you’d offer anyone you love.
Healing starts when we stop punishing ourselves and start showing kindness to ourselves instead.